国家知识产权局宣布诺华重磅心衰药物中国组合物专利无效
2018-01-05 MedSci MedSci
诺华重磅心衰药物沙库巴曲缬沙坦钠片遇挫。1月3日,国家知识产权局专利复审委员会发布诺华重磅药物Entresto(沙库巴曲缬沙坦钠片,LCZ696)的专利审查结果:专利权人诺华股份有限公司的发明创造《含有缬沙坦和NEP抑制剂的药物组合物》“宣告专利全部无效”。Entresto是一种治疗心衰的药物,2015年7月获得了美国FDA批准上市,同年11月获得欧盟批准。2016年2月,诺华向中国国家食品药品监
诺华重磅心衰药物沙库巴曲缬沙坦钠片遇挫。1月3日,国家知识产权局专利复审委员会发布诺华重磅药物Entresto(沙库巴曲缬沙坦钠片,LCZ696)的专利审查结果:专利权人诺华股份有限公司的发明创造《含有缬沙坦和NEP抑制剂的药物组合物》“宣告专利全部无效”。
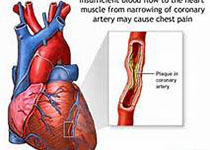
Entresto是一种治疗心衰的药物,2015年7月获得了美国FDA批准上市,同年11月获得欧盟批准。2016年2月,诺华向中国国家食品药品监督管理总局(CFDA)提交了上市申请,同年12月被CDE以“与现有治疗手段相比具有明显治疗优势”的理由纳入了优先审评。
去年7月,诺华宣布Entresto(沙库巴曲缬沙坦钠片,LCZ696)正式获得CFDA批准在中国上市,用于射血分数降低的成人慢性心衰患者,以降低其心血管死亡和心衰住院的风险。
2017年4月,广东胜伦律师事务所合伙人、律师戴锦良向专利复审委员会提出上述专利无效宣告请求,理由是“涉案专利说明书公开不充分”,“权利要求得不到说明书的支持”,“权利要求保护范围不清楚”,“权利要求不具备创造性”,不符合专利法相关条款。
戴锦良发起的这一无效宣告请求被列为专利复审委员会“重大案件公开审理”的第五例案件,于2017年9月15进行了公开审理。知识产权局在网站发布信息称,“该案的无效宣告请求理由涉及缺乏实验数据致使说明书公开不充分、申请日后提交的实验数据以及药物的协同作用等药物发明专利领域的焦点问题,极具看点。”
这一相关药物也是国内众多企业意欲角逐的领域。国家食药总局药品审评中心显示,针对沙库巴曲缬沙坦钠片,四川青木制药、成都苑东生物制药申请化药2.1类新药临床试验申请,受理号分别为CXHL1700256、CXHL1700257、CXHL1700258。
今日,知识产权局会发布了审查结果,不过诺华依然拥有向北京知识产权法院起诉的权利。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心衰药物#
39
#诺华#
33
#重磅#
31
#知识产权#
0
学习了受益匪浅
54