Cell Stem Cell:脂质代谢是癌干细胞的潜在致命弱点
2017-01-07 佚名 生物谷
在一项新的研究中,来自美国普渡大学、西北大学和印第安纳大学的研究人员发现一种代谢特征对启动肿瘤形成的“癌干细胞”的正常运转是至关重要的。他们也证实如何干扰卵巢癌中的这种代谢机制,从而抑制肿瘤生长。相关研究结果于2016年12月29日在线发表在Cell Stem Cell期刊上,论文标题为“Lipid Desaturation Is a Metabolic Marker and Therapeut

论文共同通信作者、普渡大学韦尔登生物医学工程学院Ji-Xin Cheng教授说,“这些癌干细胞抵抗常规的疗法,而且导致化疗之后的肿瘤复发和远距离肿瘤转移产生。理解它们的独特特征和弱点将能够开发出靶向疗法,从而实现克服肿瘤复发和转移的终极目标。”
这项新的研究着重关注利用抑制执行一种被称作脂质分子“去饱和作用”的代谢过程所需的酶的活性来靶向癌干细胞。
Cheng说,“癌干细胞中的不饱和脂质在维持它们发挥功能所需的信号中起着非常重要的作用。科学家们对癌干细胞有所了解,但是这些细胞中的脂质代谢是一种非常新的课题。理解癌干细胞中的脂质代谢为癌症检测和治疗提供一种新的方法。”
论文共同第一作者、普渡大学博士后研究员Junjie Li说,“在这项研究中,我们对单个活细胞进行化学成像,首次鉴定出和描述卵巢癌干细胞中的脂质不饱和性。”另一名论文共同第一作者是西北大学费恩柏格医学院助理教授Salvatore Condello。
研究人员证实一种特异性的“信号通路”直接调节被称作脂肪酸去饱和酶的脂质酶的产生。
Cheng说,“总而言之,我们的发现揭示出增加的脂质不饱和性是卵巢癌干细胞的一种代谢标志物,也是靶向它们的一种治疗靶标。”
论文共同通信作者、西北大学费恩柏格医学院Daniela Matei教授说,鉴定出独特的代谢特征是向前迈出的重要一步。这些代谢特征能够被作为清除癌干细胞的致命弱点。
她说,“我们在这项研究中提出一种根除在进行标准治疗后导致肿瘤复发的癌干细胞的全新策略,并且阐明脂质代谢如何促进卵巢癌干细胞存活。”
在此之前,缺乏灵敏的单细胞分析工具限制了对癌干细胞代谢活性的描述。用于这项研究中的成像方法是由Cheng团队开发的,允许科学家们检测单个细胞中的代谢特征。鉴于癌干细胞是癌细胞群体中的极小一部分,因此在检测隐藏的代谢特征时,单细胞灵敏度是非常重要的。
这种新的成像方法采用了两种技术:对单个活细胞进行高光谱受激拉曼散射成像(hyperspectral stimulated Raman scattering imaging)和对提取出的脂质进行质谱分析。
Cheng说,“我们在这项研究中报道相比于非癌干细胞,卵巢癌干细胞中的不饱和脂质水平显著增加。常规方法并不能够开展单细胞分析。如果这种特征存在于一个非常小的区域,那么它不容易被常规生化测试方法检测到。利用受激拉曼显微分析法,我们能够更好地通过这种代谢特征精确地找到这些细胞。”
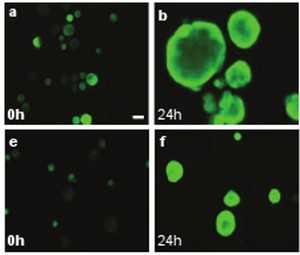
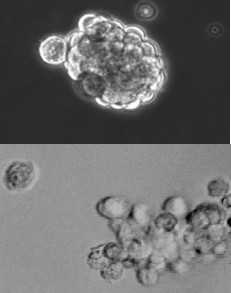
这种脂质不饱和性特征是在实验室培养的卵巢癌干细胞和来自卵巢癌病人的细胞中鉴定出来的。更高的脂质不饱和性水平也在利用癌干细胞培养出的模拟病人体内肿瘤组织的三维“球状体(spheroid)”中检测到。研究人员利用一种化学物抑制脂肪酸去饱和酶的活性,降低这些细胞的“干性(stemness)”,使得它们变得不那么致命性。Cheng说,抑制脂肪酸去饱和酶的活性有效地清除癌干细胞,阻止实验室培养物中的球状体形成和阻断实验室小鼠体内的肿瘤起始能力。
Li说,“我们并不直接地阻断这种信号通路,我们阻断脂肪酸代谢以至于这些不饱和脂质水平下降,这实际上抑制这些癌干细胞的功能。”
Junjie Li10, Salvatore Condello10, Jessica Thomes-Pepin, Xiaoxiao Ma, Yu Xia, Thomas D. Hurley, Daniela Matei, Ji-Xin Cheng.Lipid Desaturation Is a Metabolic Marker and Therapeutic Target of Ovarian Cancer Stem Cells.Cell Stem Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
31
#stem cell#
26
#Cell#
25
#脂质代谢#
38
#STEM#
33
#癌干细胞#
27
这项研究的意义还是非常重大的,但是能不能找到脂代谢的靶点还是个问题
44
厉害我的哥
40