Nat Commun:通过基因异构体比率预测癌症病人生存期更有效
2016-06-14 MedSci MedSci原创
来自加州大学洛杉矶分校(UCLA)邢毅教授领导的团队提出了癌症生存期分析的新统计算法SURVIV。 SURVIV(Survival analysis of mRNA isoform variation)利用肿瘤样本高通量RNA测序(RNA-Seq)数据,通过考虑基因异构体定量的不确定度来评估生存时间与基因异构体比率的相关性。相关成果发表在6月9日的《Nature Communications》(
来自加州大学洛杉矶分校(UCLA)邢毅教授领导的团队提出了癌症生存期分析的新统计算法SURVIV。
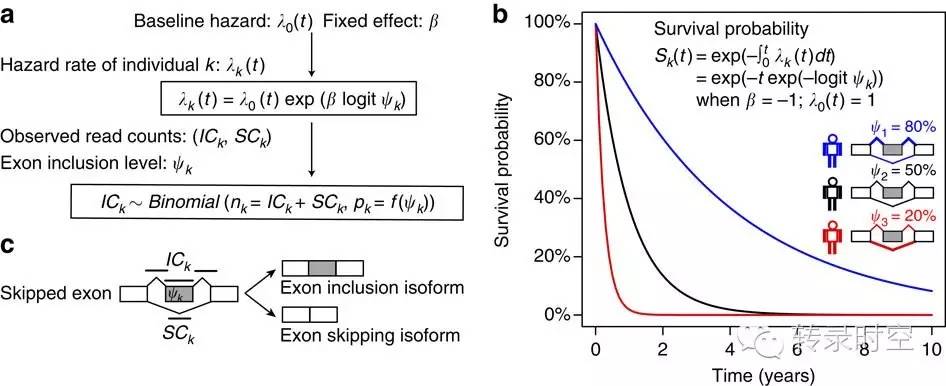
SURVIV(Survival analysis of mRNA isoform variation)利用肿瘤样本高通量RNA测序(RNA-Seq)数据,通过考虑基因异构体定量的不确定度来评估生存时间与基因异构体比率的相关性。相关成果发表在6月9日的《Nature Communications》(自然:通讯)上。
他们利用SURVIV 分析了近700例癌症基因组图谱(TCGA)数据库乳腺浸润性导管癌样本,结果显示:无论是真实数据还是模拟数据,SURVIV的分析结果比不考虑异构体定量的不确定度的分析结果更加准确,尤其是在没有深度测序数据的情况下,该方法的表现更为出色。
一旦与临床数据和基因表达量数据结合,该方法则显现出更强的预测精度。他们还发现,在只有RNA-Seq数据的情况下,利用基因异构体预测生存期比利用基因表达量预测在6种不同的癌症中结果都好。
以往针对不同组织的RNA-Seq研究表明,人类基因在特定情况或不同组织中,呈现不同的剪接形式从而产生不同的基因异构体。有证据表明,可变剪接在癌症的发生发展过程发挥一系列作用,包括肿瘤形成、转移、免疫逃逸等。
与过去的研究往往通过比较癌症和正常组织样本,寻找癌症特异的剪接事件不同的是,他们是第一个从大量肿瘤样本里寻找生存期相关的剪接事件的研究团队。
为了证明可变剪接与癌症生存期的相关性,他们首先运用SURVIV研究外显子遗漏(exon-skipping,可变剪接的其中一种类型)在6种癌症类型中的情况。利用一系列不同测序深度的600例乳腺癌模拟数据,他们发现SURVIV寻找到的基因异构体比不考虑异构体定量不确定度的Cox回归生存分析更准确。随着测序深度降低,SURVIV方法就变得更加有优势。
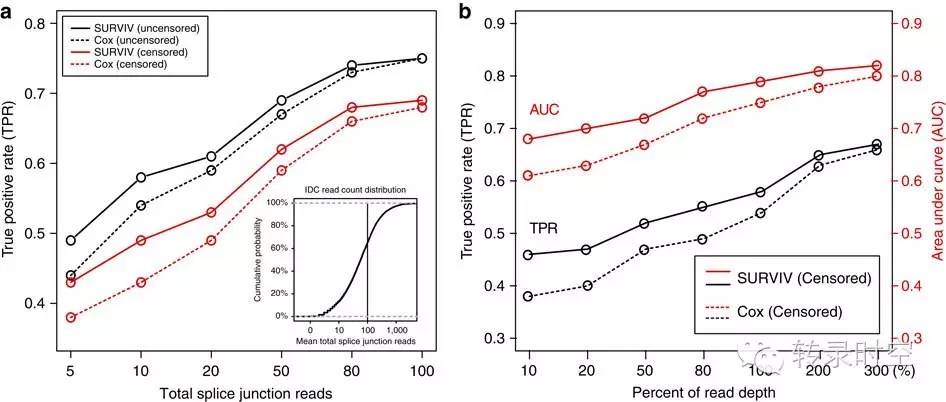
“通过考虑异构体定量的不确定度,我们可以得到更加可靠的估计,尤其当测序覆盖度不是很高的情况下。这种情况在临床样本数据中很常见”,邢毅说,“我们对每个样本的最深覆盖度模拟达到2亿条序列,很少有RNA-Seq的数据能达到这样的深度。TCGA数据库的RNA-Seq数据集,其测序深度一般只有这个深度的四分之一”。
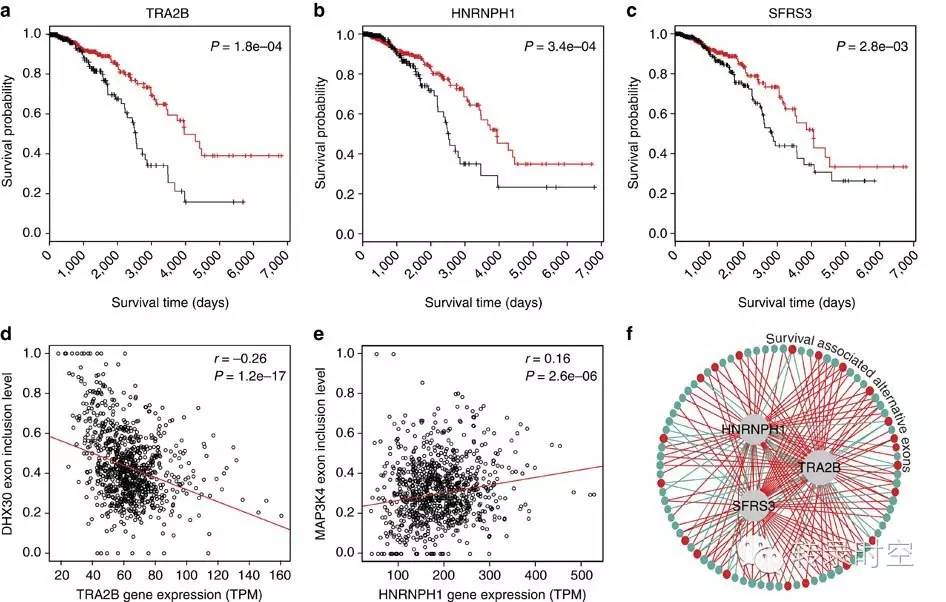
在TCGA数据库682例乳腺浸润性导管癌样本的真实数据里,该算法可找到229个外显子遗漏事件与病人的生存时间高度相关。这些发生外显子遗漏的基因很可能在癌症细胞里发挥了作用,比如转录因子、DNA损伤应激基因、氧化和凋亡通路有关的基因等。他们并不认为所有这些基因对癌症都有直接作用。但他们相信,这些生存相关的可变剪接事件对理解肿瘤的发生发展和易感性,提供了新的思路。
姚军( Jun Yao,音译),一位来自美国得克萨斯大学MD Anderson癌症研究中心的神经肿瘤学研究学者, 评论说下一步着手研究这些外显子遗漏事件的生物学结果会很有意义。姚军已经对肿瘤特异异构体和可变剪接研究了很多年了。他认为,用SURVIV来预测癌症生存期是“一个很新颖有趣的方法”。当然,更多的实验验证和后续的功能性研究能帮助排除该方法得到的假阳性结果。
UCLA的研究团队也希望通过基因异构体比率的分析,可以找到具有临床诊断价值的分子标记物。他们发现,从乳腺癌数据中找到的外显子遗漏事件,可以用作肿瘤分型。他们还鉴定出3个可变剪接调控因子,可能对84个与生存时间相关的外显子遗漏事件进行直接调控。这其中之一就有已经被报道过的TRA2B基因,它在某些乳腺癌中高表达。
邢毅和他的团队希望研究更多的癌症类型和更大规模的数据,也希望与更多临床研究人员合作。“通过SURVIV的结果,我们可以预测癌症生存期,”邢毅说,“接下来我们可以尝试利用这些基因异构体比率特征来预测病人对药物治疗的反应。这应该很具有临床意义和商业价值。”
“虽然现在我们的研究集中在外显子遗漏这一种可变剪接类型上,”邢毅说,“SURVIV其实是可以分析所有可变剪接类型的”。他还补充说,他们正在开发能整合更多临床变量的新模型。
参考文献:
Shen S, Wang Y, Wang C, Wu YN, Xing Y. SURVIV for survival analysis of mRNA isoform variation. Nat Commun. 2016 Jun 9;7:11548. doi: 10.1038/ncomms11548.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#预测癌症#
41
#Nat#
34
#COMMUN#
39
#生存期#
25
第一个抢沙发,学习了
90