JCB:糖尿病药物罗格列酮可打破卵巢癌的保护性壁垒
2016-12-04 MedSci MedSci原创
Rice大学的科学家们在Journal of Cellular Biochemistry杂志上发表文章指出,糖尿病药物可以瓦解肿瘤的保护性壁垒。我们体内的细胞和器官上有一层糖蛋白组成的保护性粘液。肿瘤可以操纵这些糖蛋白,帮助自己躲避化疗和免疫系统的攻击。研究人员发现,噻唑烷二酮类药物可以阻止这种糖蛋白的表达。“我们感兴趣的高分子量糖蛋白能吸收水分,覆盖并保护在细胞表面,” Rice大学的Danie
Rice大学的科学家们在Journal of Cellular Biochemistry杂志上发表文章指出,糖尿病药物可以瓦解肿瘤的保护性壁垒。
我们体内的细胞和器官上有一层糖蛋白组成的保护性粘液。肿瘤可以操纵这些糖蛋白,帮助自己躲避化疗和免疫系统的攻击。研究人员发现,噻唑烷二酮类药物可以阻止这种糖蛋白的表达。
“我们感兴趣的高分子量糖蛋白能吸收水分,覆盖并保护在细胞表面,” Rice大学的Daniel Carson说。“这些粘蛋白(mucin)排列在口腔、腺体和胃肠道,具有非常重要的保护性功能。”肿瘤将这些蛋白作为自己的表面屏障,使免疫细胞无法接触和杀伤癌细胞。如果能够减少患者的粘蛋白水平,宿主免疫系统也许就能杀死肿瘤。
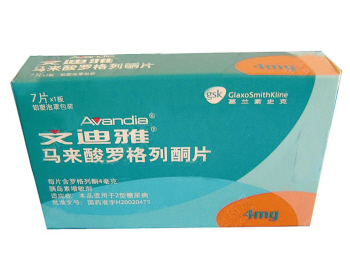
研究人员分析了噻唑烷二酮类药物PPARγ罗格列酮(Rosiglitazone )对糖蛋白MUC16的影响,MUC16保护着乳腺癌和卵巢癌细胞。“我们对MUC16特别感兴趣,因为它也称为CA125,是卵巢癌的经典标志物,” Carson说。女性血液中的CA125水平一般非常低,但卵巢癌细胞会释放CA125。
肿瘤微环境中有很多细胞因子。人们一直认为这些促炎症介质是好东西,因为它们可以增强抗肿瘤的免疫应答。但研究人员发现,它们也增强了肿瘤的保护性应答,提高了癌细胞的MUC16生产。研究显示,罗格列酮能干扰细胞因子的作用,关闭癌细胞的糖蛋白生产。
MUC16生产中止几天,癌细胞的保护性屏障就会被突破,免疫细胞就能开始摧毁肿瘤。不过,在用糖尿病药物治疗癌症之前还有很多问题需要解决。举例来说,罗格列酮只有在大剂量直接作用于肿瘤的时候才有效。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#罗格列酮#
47
#糖尿病药物#
38
学习了好东西!
78
太神奇啦!这是真的吗?
67
学习了,很好!
67
学习中…………
71
继续学习
66
继续关注
35