Nat Genet:遗传meta分析揭示胶质瘤与非胶质瘤的分子奥秘
2017-04-04 MedSci MedSci原创
一项大规模遗传meta分析,荟萃了包括30,000多人血液样本的大规模研究成果,通过这项分析,研究人员确定了13种胶质瘤新遗传危险因素,这揭示了增加胶质瘤易感性的个体DNA的特殊差异,同时也首次为临床医师提供了一种能区分成胶质细胞瘤和非胶质母细胞瘤等胶质瘤类型的新方法。这一研究成果公布在3月27日的Nature Genetics杂志上。脑胶质瘤由神经上皮细胞恶化演进形成,是成人中枢神经系统中最常见
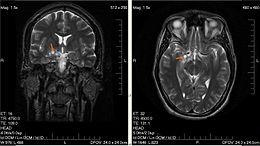
脑胶质瘤由神经上皮细胞恶化演进形成,是成人中枢神经系统中最常见的恶性肿瘤,致死率极高,恶性脑胶质瘤5年存活期仅5%,具有浸润生长、易复发、预后差等特点。根据WHO形态学分类标准,脑胶质瘤分为四个级别和多种类型,其恶性程度不同,常规放化疗的预后差别较大,不同分型以及原发和复发胶质瘤发生发展的分子机制也有所不同,因此亟需发展针对分子病理的新的分型标准,指导临床治疗和个体化医疗,提高病人的生存期和生存质量。
文章作者,凯斯西储大学医学院综合癌症中心 Jol Barnholtz-Sloan博士说:“由于这项研究中使用的样品量很大,因此我们能第一次评估出胶质母细胞瘤与非胶质母细胞瘤的遗传风险是否不同。结果显示它们的遗传风险特征确实不同。
这项大规模研究由来自瑞典,丹麦,英国,德国,加拿大和以色列等20多个机构的63位作者完成,Barnholtz-Sloan说:“胶质瘤虽然是成年人最常见的恶性脑肿瘤类型,但样品并不容易找到,因此为了找到具有科学有效性的样本量,我们需要多机构合作。”
在新研究中,研究人员分析了多个已发表的全基因组关联研究GWAS数据。GWAS目前成为了许多实验室采用的研究工具,可以用于搜索与疾病风险相关区域的DNA序列数据。这些研究确定了患者体内的特定DNA序列分子,如G,C,T或A的变化。之前的研究曾确定了13个特殊DNA位置会增加发生胶质瘤的风险。而新研究将这个数字翻了一番,确定了另外13个新的基因位置,其中5个属于胶质母细胞瘤,8个属于非成胶质细胞瘤。
Barnholtz-Sloan说:“通过meta分析 ,我们从最可靠的研究入手,”总共来说,这个研究小组分析了来自12,496人的胶质瘤(6,191个胶质母细胞瘤和5,819个非成胶质细胞瘤),以及18,190个无胶质瘤患者的数据。
新确定的遗传危险因素有助于区分最有可能发展成各种胶质瘤的患者。根据美国脑肿瘤协会的报道,每种肿瘤亚型都有不同的预后,最常见的是胶质母细胞瘤,仅有12-14个月的中位生存期(median survival)。通过这项新研究,临床医师们能够更早地诊断高危患者,从而最终改善其预后效果。
梅斯医学小编为您再拓展一些:
基于遗传的meta分析是重要的工具,有很多重量级成果发表。在一项多达10万人(包括17,000名最常见类型的卵巢癌患者)的遗传分析研究中,研究人员确定了12种新的增加卵巢癌患病风险的遗传变异,并找到了它们与以前发表的18种变异之间的关联。(Nat Genet:大规模研究发现可能增加卵巢癌风险的新变异)
2015年,一篇刊登于国际著名杂志Nature Genetics上的研究报告中,来自哥伦比亚大学等处的科学家通过研究发现了15个新型的“热点区域”,其可以增加女性患乳腺癌的风险;文章通过meta分析对比了超过12万患乳腺癌或不患乳腺癌的欧洲女性机体的遗传组成的微小变化,最终鉴别出了15个名为单核苷酸多态性(SNPs)的突变,其和乳腺癌风险升高直接相关。这项新型研究发现就意味着目前研究人员发现了超过90个SNPs和乳腺癌发病直接相关。其中两个主要的靶基因区域为 SETBP1 at 18q12.3 和RNF115 and PDZK1 at 1q21.1(Nat Genet: 新发现乳腺癌15个高风险SNP位点(meta分析)
2012年12月25日之前发表的有关结直肠癌与遗传变异相关性的论文,对其中910篇论文进行了Meta分析,共涉及150个候选基因中的267个遗传变异体的。使用威尼斯标准和假阳性报告率评价其结直肠癌风险相关的累积流行病学证据等级。结果发现,共有62个变异体与结肠直肠癌风险显著相关。结直肠癌风险相关的累积流行病学证据分为三个等级:5个基因(APC、 CHEK2、DNMT3B、MLH1和MUTYH)中有8个变异体属于强度 ;2个基因中的2个变异体属于中度;45个基因中的52个变异体属于低度。(Gut:Meta分析揭示结直肠癌相关遗传变异位点)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gene#
25
#MET#
32
#NET#
21
#Meta#
25
#Genet#
31
#Nat#
23
很好的研究
75
看看了解一下
40
好东西学习了!
58
现代医学已经从组织器官医学发现为分子生物学,技术发展是科学的桥梁!
71