科学家建议把比传统成像更准确的分子成像技术引入常规临床实践。
《柳叶刀》发表的一篇新文章称,一种名为PSMA PET/CT的医学成像技术能够提供前列腺癌相关分子水平以及详细的全身分布,可帮助医生确定疾病的扩散程度。这篇文章报告了来自澳大利亚300名患者的随机对照试验结果。
这种方法结合了正电子发射断层扫描(PET)和计算机断层扫描(CT)两种成像技术,据报道,用这种方法在精确定位前列腺癌在体内扩散情况的准确率比现有的标准成像方法高出近三分之一:PSMA PET/CT的准确率为92%,标准成像的准确率仅为65%。
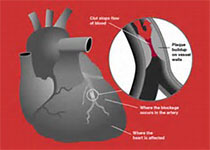
手术切除或者强化放疗是前列腺癌的常见治疗方法。但是如果癌症已经扩散到身体的其他部分了,医生就需要根据CT和骨骼扫描来确定是否需要额外的治疗。
这种方法用一种放射性物质检测患者体内的前列腺特异膜抗原(Prostate Specific Membrane Antigen,PSMA),然后进行PET/CT扫描,CT扫描照射出人体器官和结构,PET扫描高亮哪些区域存在高水平的PSMA,提示前列腺癌细胞所在位置。
试验发现,传统影像学检测未能发现29名患者癌症已经扩散,结果呈假阴性,而PSMA PET/CT的假阴性结果仅为6例,此外,新技术的假阳性有2例,而传统影像学的假阳性有9例。
虽然两种方法都有辐射,但PSMA PET/CT的辐射剂量小于常规成像的一半。
“大约三分之一前列腺癌患者在手术或放疗后复发,这在一定程度上是因为现在的医学成像技术常常判断不出来癌症是在什么时候扩散的,意味着一些患者没有及时得到额外治疗。PSMA PET/CT可以帮助患者们更快得到适当治疗,”文章通讯作者Declan Murphy教授说。
原始出处:Prof Michael S Hofman, Nathan Lawrentschuk, Roslyn J Francis, MBBS et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multi-centre study. Lancet. March 22, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
32
#新分子#
44
#侵袭性#
33
#成像技术#
41