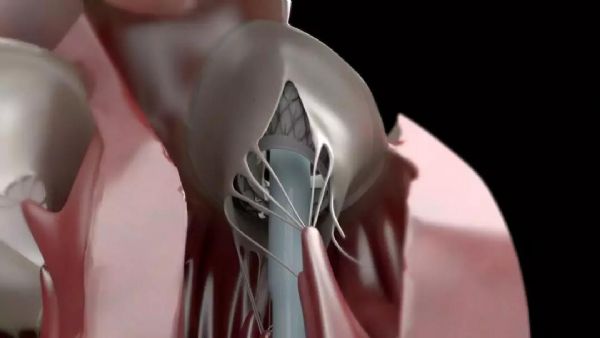
中山医院王春生教授团队成功实施亚洲首例经导管二尖瓣置换术
2019-05-29 不详 复旦大学附属中山医院
72岁的徐奶奶3年来反复出现活动后胸闷气急、夜间阵发性呼吸困难、双下肢严重水肿、房颤、频发室性早搏,在多家医院采取内科保守治疗均无效,万般无奈之下,徐奶奶来到复旦大学附属中山医院就诊,心超确诊为二尖瓣前叶大范围脱垂伴重度反流,左心室内径显著扩大至77 mm,LVEF降低为49%,心衰标志物NT-proBNP高达13072 pg/ml。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#二尖瓣置换术#
41
#经导管二尖瓣置换术#
36
#置换#
25
#中山医院#
46
#二尖瓣#
33
#经导管#
22
#置换术#
21
学习了,谢谢分享
46