老年患者腹部大手术后2天左肺不张,夜间紧急予以气管镜吸痰,医生忠告--胸腹部大手术后不要忘记气道廓清,否则后果严重!
2022-08-14 呼吸科的故事 呼吸科的故事
围手术期的管理很重要,其中呼吸道的管理尤为重要,采取有效措施帮助患者排出痰液,密切监测患者症状及体征变化,及时与相关科室联系,处理好并发症,保障患者安全。
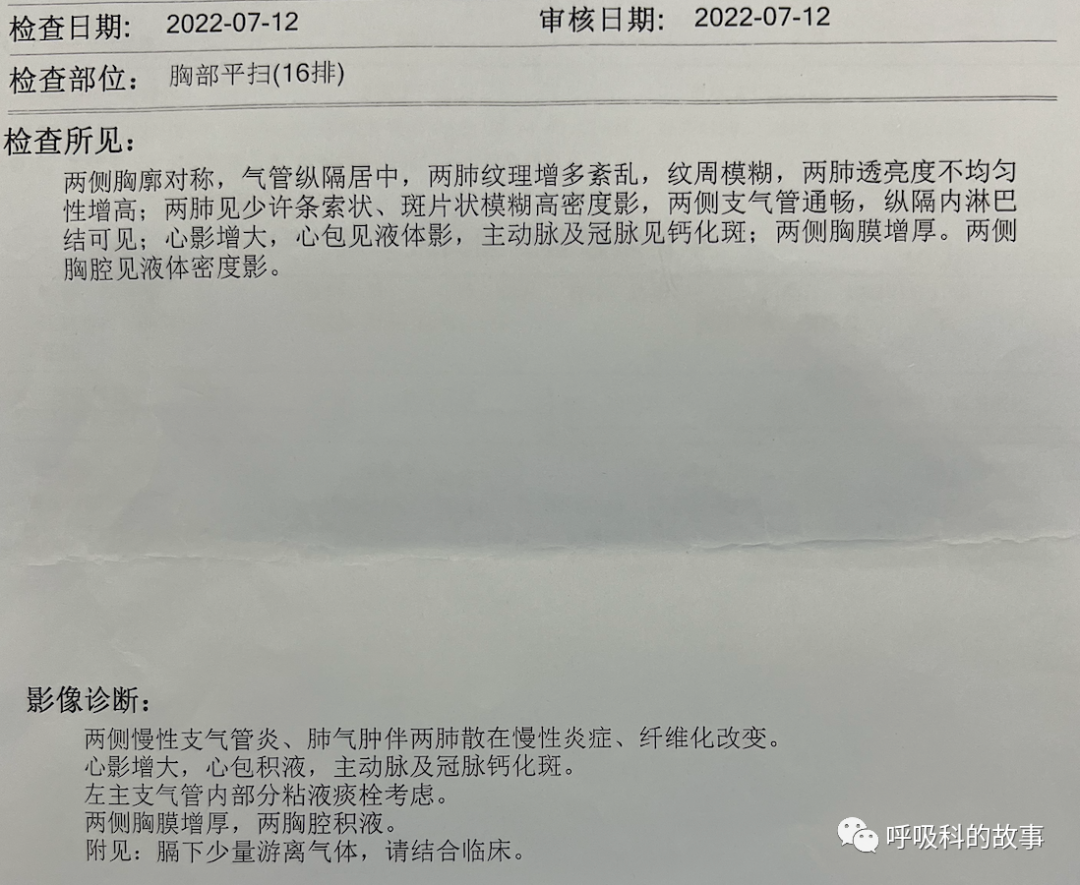
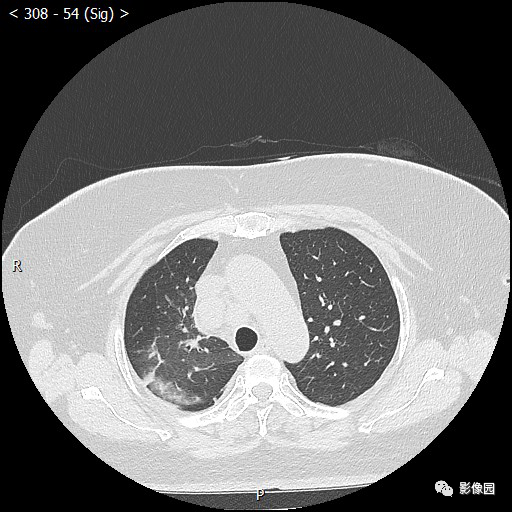
昨天夜班,急诊室来了一个从杭州某县医院转诊过来的患者。患者是72岁老伯,因为胃穿孔紧急行手术治疗,术后患者高热转到我院。入院前在当地医院做过一次肺部CT(2022-7-12),报告如下:
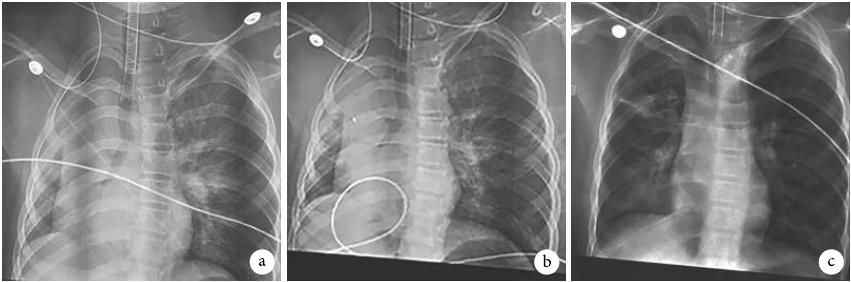
在急诊科查体发现左肺呼吸音明显减低,于是立即行肺部CT,医生们惊讶地发现患者的左肺全肺不张,立即请笔者会诊。
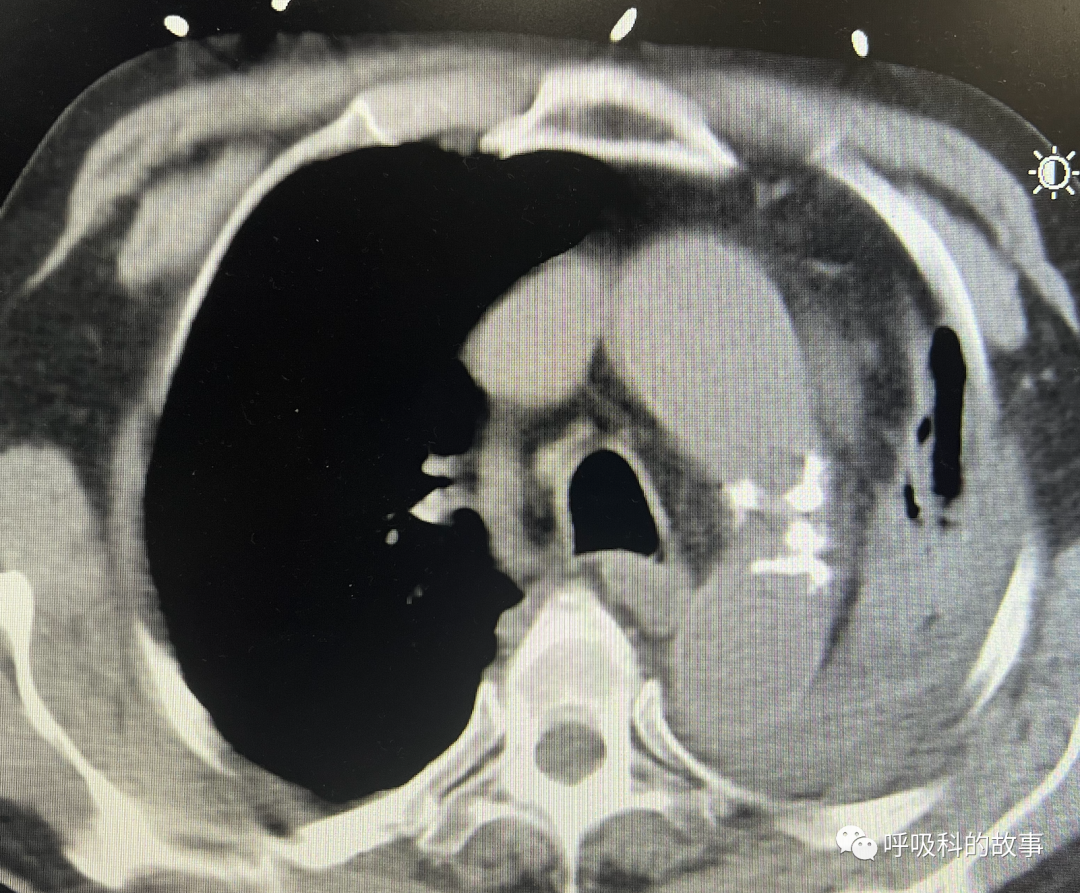
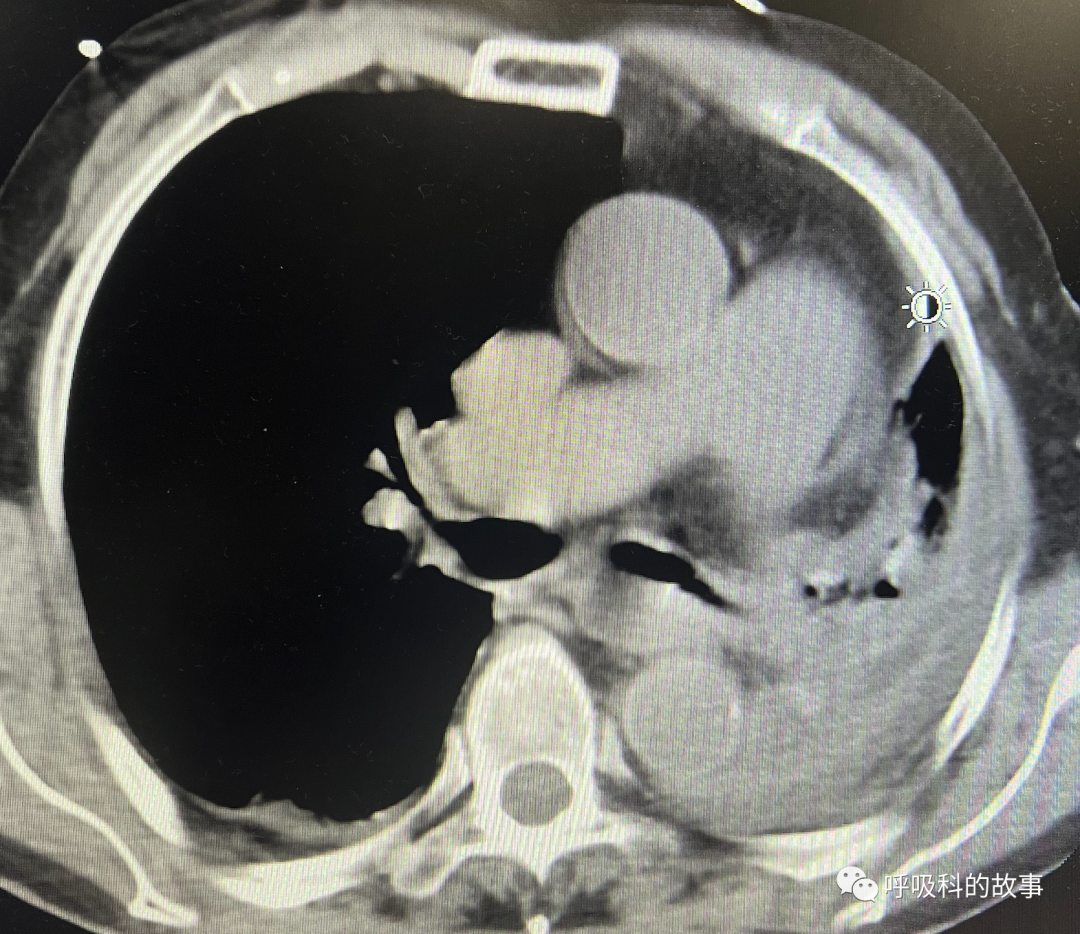


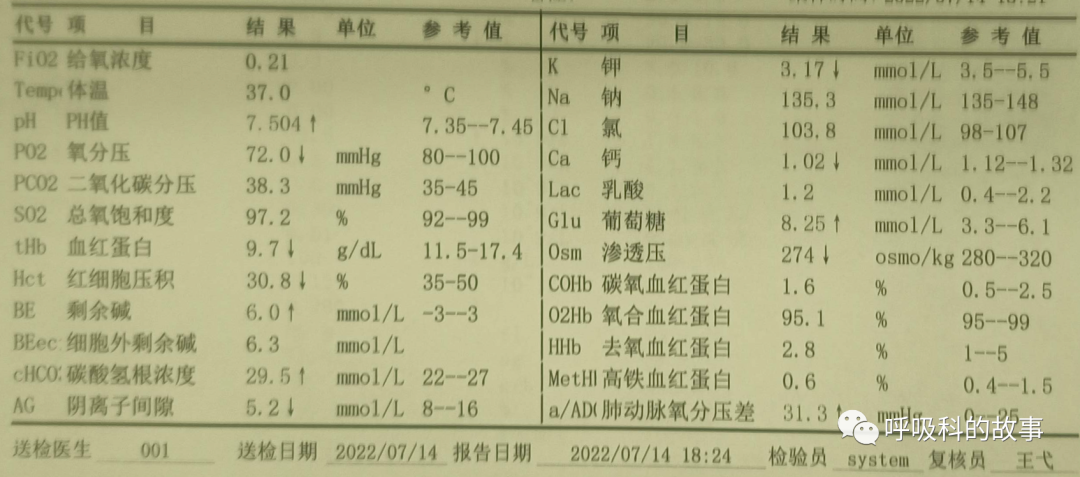
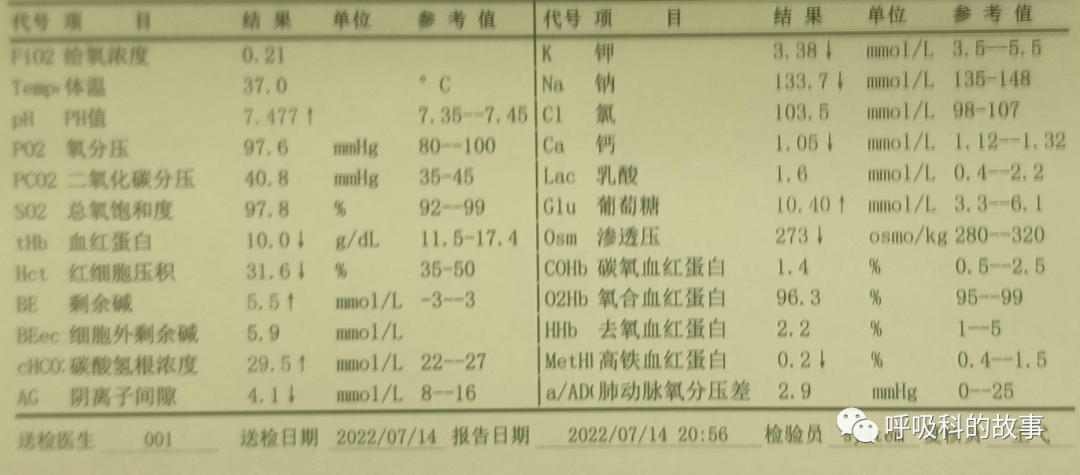
笔者先了解患者情况,得知患者平时就有咳嗽、咯痰,术后因为腹部切口疼痛不敢咳嗽,咯痰量很少,家属也因为害怕加剧患者的疼痛仅轻轻拍背。于是,笔者推测患者左肺全肺不张是气道内大量痰栓堵塞气道所致的,而且患者血气提示低氧血症,因此要立即通过气管镜予以吸取痰栓。
于是,笔者在急诊科同仁的协助下于床边行气管镜检查,可见气道内大量粘稠痰栓将左主支气管及左侧各级支气管完全堵塞,还伴有黄色胆汁,反复吸取,经过近20分钟的努力终于将气道内痰栓清除干净。
气管镜检查后,复查床边胸片,左肺复张,血气结果也有明显改善:

笔者反复交待患者和家属,即使因为切口疼痛,也要在医生镇痛药物的帮助下,尽可能学习如何有效地咳嗽排痰。同时,笔者也想对外科同行说:围手术期的管理很重要,其中呼吸道的管理尤为重要,采取有效措施帮助患者排出痰液,密切监测患者症状及体征变化,及时与相关科室联系,处理好并发症,保障患者安全。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#吸痰#
43
#肺不张#
45
#大手术#
34
#紧急#
30
#左肺#
28