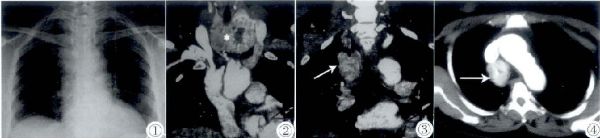
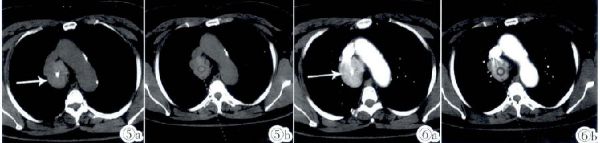
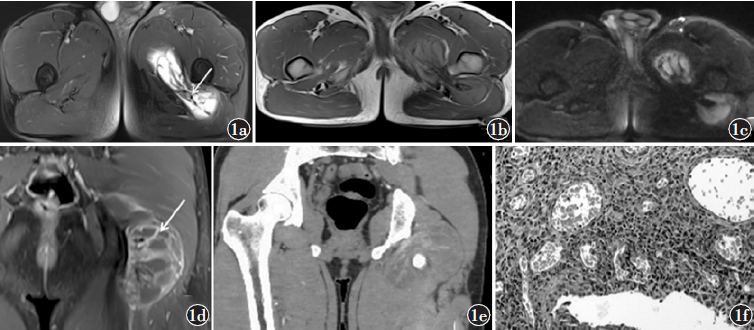
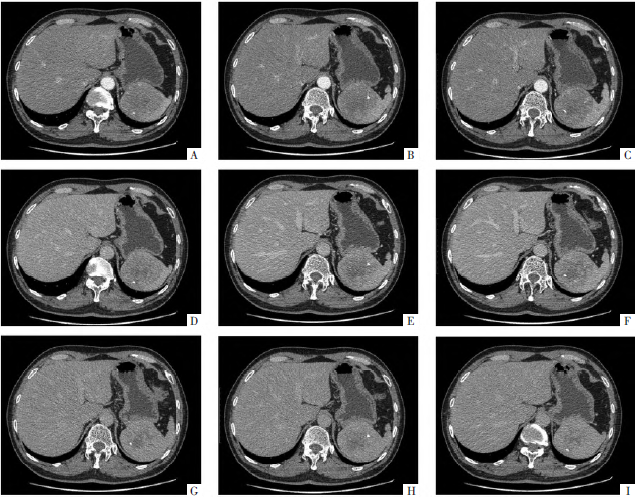
结节性甲状腺肿伴微乳头状癌合并中后纵隔异位甲状腺1例
2019-05-09 马伟伟 周子恩 洪鸣 中国临床医学影像杂志
病例女,63岁,2009年4月因咳嗽于外院就诊。查体:心肺未见异常。患者无其它不适。既往体健,有高血压病史5年(口服降压药控制良好),无吸烟饮酒史,否认放射性物质及有害有毒物质接触史,近半年体质量无明显变化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#甲状腺肿#
40
#后纵隔#
50
#结节性#
40
#中后纵隔#
45
#乳头状#
42