Blood:BH3图谱分析发现ruxolitinib可与ventoclax联合治疗前体T淋巴细胞白血病
2021-02-20 MedSci原创 MedSci原创
HDAC和JAK/STAT通路抑制剂是ventoclax的有前景的联合用药选择
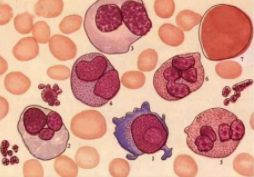
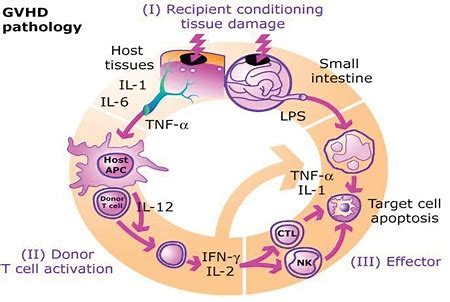
前体T淋巴细胞白血病(T-PLL)的常规治疗方法,如细胞毒性化疗和阿仑单抗(阿仑单抗),疗效有限,且毒性较大。一些新的药物类别已经在T-PLL中显示出了临床前活性,包括JAK/STAT和TCR通路的抑制剂,以及组蛋白去乙酰化酶(HDAC)抑制剂。近期,BCL-2抑制剂ventoclax也在T-PLL中显示出了一定的临床活性。
Herbaux等人尝试表征T-PLL的功能性凋亡依赖性,以确定治疗这种疾病的新的联合疗法,研究结果于近日发表在《血液》“Blood”杂志上。
BH3图谱分析是一种评估细胞凋亡倾向(“启动”)和细胞对不同抗凋亡蛋白的相对依赖性的功能性分析方法。
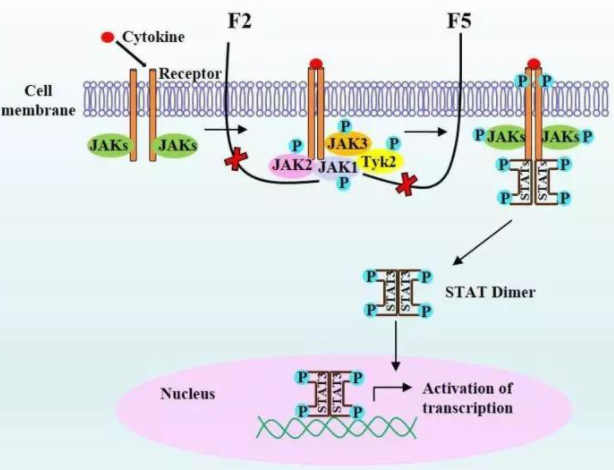
Herbaux等人对24例原发性T-PLL患者的样本进行了BH3图谱分析发现,原代T-PLL细胞的凋亡启动水平相对较低,主要依赖BCL-2和MCL-1存活。选择性药物抑制BCL-2或MCL-1可诱导原代T-PLL细胞死亡。用JAK1/2抑制剂鲁索替尼(ruxolitinib)靶向JAK/STAT通路,或用贝利司他(belinostat )靶向HDAC,均可独立增加T-PLL细胞对BCL-2的依赖(但不改变对MCL-1的依赖性),从而增强了T-PLL细胞对ventoclax的敏感性。
基于上述结果,研究人员采用ventoclax联合鲁索替尼治疗了两例难治性T-PLL患者:JAK3突变的T-PLL患者获得了的深度缓解,无突变患者病情表现稳定。
综上,本研究基于精准医学的功能性方法明确了HDAC和JAK/STAT通路抑制剂是ventoclax的有前景的联合用药选择,值得开展T-PLL相关临床试验进一步探索这种联合方案。
原始出处:
Charles Herbaux, et al. BH3 profiling identifies ruxolitinib as a promising partner for venetoclax to treat T-cell prolymphocytic leukemia. Blood. February 17, 2021. https://doi.org/10.1182/blood.2020007303
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#淋巴细胞白血病#
49
#T淋巴细胞白血病#
32
#淋巴细胞#
42
#联合治疗#
37
#ruxolitinib#
37
#T淋巴细胞#
43
学习了!
90