CELL: 研究揭示一种肠道代谢物与CVD相关
2020-03-17 idiabetes idiabetes
来自克利夫兰诊所的一个研究小组发现了一种肠道微生物副产物,这种副产物在临床和机制方面均与心血管疾病(CVD)有关。这种名为苯乙酰谷氨酰胺(PAGln,简称PAG)的代谢物已被证实通过肾上腺素能受体发挥
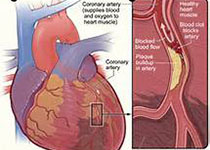
来自克利夫兰诊所的一个研究小组发现了一种肠道微生物副产物,这种副产物在临床和机制方面均与心血管疾病(CVD)有关。这种名为苯乙酰谷氨酰胺(PAGln,简称PAG)的代谢物已被证实通过肾上腺素能受体发挥作用,导致血小板活性和聚集增强,并在体内形成血栓。
克利夫兰诊所Stanley Hazen研究团队在3月5日《细胞》杂志上发表了他们的发现。他表示,PAG这种由肠道微生物产生的化合物似乎可以调节肾上腺素受体,并认为这正是其与许多心血管表型和疾病紧密联系的原因。
PAG是肠道微生物分解必需氨基酸苯丙氨酸的副产物。苯丙氨酸存在于许多植物和动物来源的蛋白中,包括肉类和豆类。Hazen称,蛋白质被消化并分解成单个氨基酸后,大部分苯丙氨酸被小肠吸收。到达大肠未被吸收的苯丙氨酸可被肠道菌群代谢,形成苯丙酮酸和苯乙酸。苯乙酸经肝脏代谢后产生PAG。控速步骤是细菌利用苯丙氨酸作为能量来源,最终生成的代谢物会转化成PAG。
研究人员使用了一个叫做非靶向代谢组学的新兴平台来识别与CVD相关的血浆代谢物。他们选择了2型糖尿病(n=1162)患者作为研究对象,因为这些患者更有可能出现与CVD相关的代谢紊乱,从而增加研究者发现新途径的可能性。
对4000例受试者的独立队列研究显示,PAG与CVD和心血管事件相关,包括心肌梗死、卒中和死亡。更有意义的是,对PAG升高的动物模型使用β受体阻滞剂可逆转PAG导致的心血管结局。此外,使用基因编辑技术或药物来阻断PAG受体信号可以显著降低凝血活性。
研究人员指出,他们发现高水平PAG促进心血管表型的出现,给予β受体阻滞剂可以逆转PAG诱导的不良表型,认为β受体阻滞剂带来的一些获益可能源自其逆转高水平PAG的效应。这是第一次用这种机制解释β受体阻滞剂的益处。
这项研究由美国国家心肺血液研究所(NHLBI)资助。NHLBI的Ahmed Hasan博士表示,Hazen团队扩展了我们对糖尿病和心脏病潜在肠道微生物群机制的了解,并展现了它们作为治疗靶标的潜力。总的来说,这项研究使用了新工具,展示了我们吃的食物是如何通过肠道微生物与健康和疾病风险联系在一起的,这可能为未来个体化的心血管疾病诊治提供帮助。
原始出处:
Nemet I, Saha PP, Gupta N, et al. A Cardiovascular Disease-Linked Gut Microbial Metabolite Acts via Adrenergic Receptors. Cell. 2020; 180(5): 862-877. e22. doi:10.1016/j.cell.2020.02.016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#代谢物#
38
#CEL#
31
#Cell#
26
学习了
77