ANN NEUROL:癌症患者凝血标志物更高,易患缺血性脑卒中
2021-10-29 MedSci原创 MedSci原创
患有活动性癌症和急性缺血性中风的患者具有更高的凝血、血小板和内皮细胞活化标记物,以及更多的循环微栓子。这表明暗示高凝和栓塞过程在实体瘤癌症患者缺血性卒中的发病机制中起作用。
据估计,4-20%的缺血性中风患者患有癌症,并且这些疾病的共患病率正在增加。这可能是由于最近癌症治疗的改进延长了患者的生存期。癌症是缺血性中风的既定风险因素。在癌症诊断后的前6个月,平均而言,癌症患者患缺血性中风的风险增加两倍。患有侵袭性癌症(如肺癌和胰腺癌)的患者和有转移的患者中,这种风险更高。癌症患者的中风往往比非癌症患者的中风更严重、更致命,且复发率更高。在标准诊断评估后,约50%的癌症相关中风被归类为隐源性中风。尽管最近的研究表明高凝状态可能起着重要作用,但对导致癌症卒中风险增加的生物学因素知之甚少。
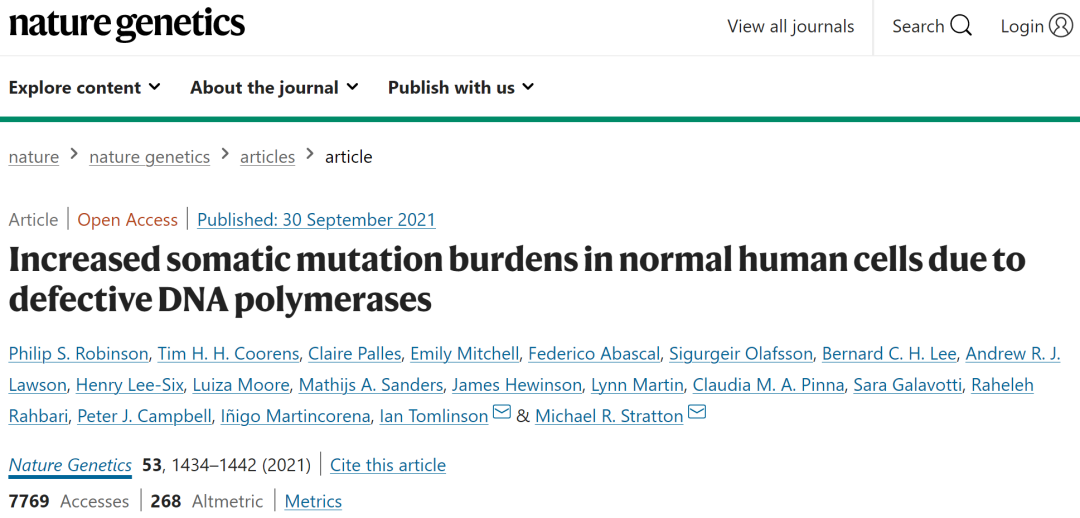
为了提高对癌症患者缺血性卒中机制的理解,Babak Navi等进行了癌症患者缺血性卒中机制(大多数癌症)前瞻性研究,比较活动性癌症缺血性卒中患者、单纯缺血性卒中患者与单纯活动性癌症患者之间凝血、血小板和内皮活化的预先指定血液学标志物以及栓塞疾病的TCD标志物。该研究发表在Annals of Neurology杂志。
该研究探讨了缺血性脑卒中合并癌症的病理生理学特点。
2016-2020年该研究小组在两家医院进行了前瞻性横断面研究。纳入了三组研究对象,每组50名成人参与者。主要组包括活动性实体瘤癌急性缺血性卒中患者。对照组仅包括急性缺血性卒中患者或活动性癌症患者。根据年龄、性别和癌症类型(如适用),将仅中风和仅癌症患者与癌症加中风患者进行匹配。测量指标是预先指定的血液学生物标志物和经颅多普勒微栓子检测。血液学生物标志物包括凝血标志物(D-二聚体、凝血酶和凝血酶)、血小板功能(P-选择素)和内皮完整性标志物(血栓调节蛋白、可溶性细胞间粘附分子-1[sICAM-1]、可溶性血管细胞粘附分子-1[sVCAM-1])。使用KruskalWallis和Wilcoxon秩和检验比较各组间的血液学生物标志物。在多变量线性回归模型中,调整了种族、卒中危险因素数量、吸烟、卒中严重程度和抗血栓药物的使用。采用卡方检验比较各组间经颅多普勒微栓子的存在情况。
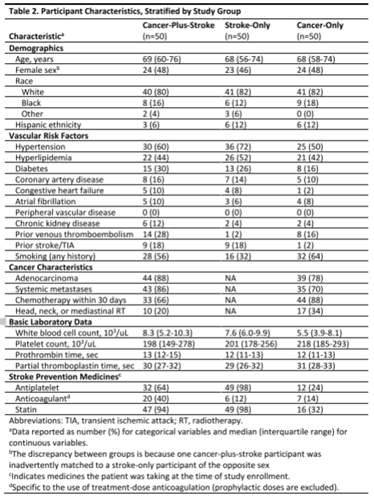
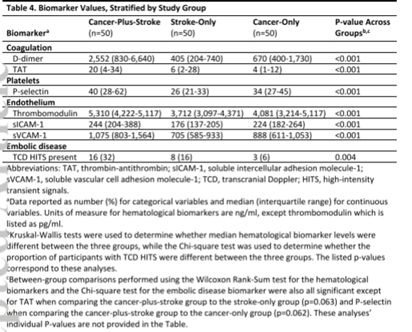
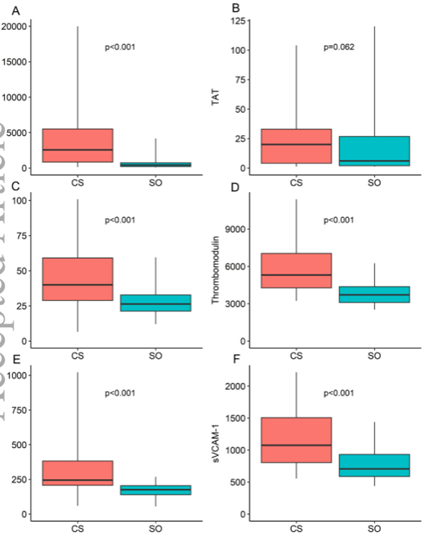
各组间所有研究生物标志物的水平不同。在单变量组间比较中,癌症合并卒中患者的D-二聚体、sICAM-1、sVCAM-1和血栓调节蛋白水平高于两个对照组;凝血酶和抗凝血酶水平高于仅癌症患者;P-选择素水平高于仅中风患者。多变量分析结果相似。32%的癌症合并卒中参与者、16%仅卒中参与者和6%仅癌症参与者检测到经颅多普勒微栓子(p=0.005)。
该研究发现与对照组相比,患有活动性癌症和急性缺血性中风的患者具有更高的凝血、血小板和内皮细胞活化标记物,以及更多的循环微栓子。这表明暗示高凝和栓塞过程在实体瘤癌症患者缺血性卒中的发病机制中起作用。
未来的研究应该评估这些生物标记物是否能够预测癌症患者发生和复发卒中的风险以及抗血栓治疗的反应。同时,临床医生应该探索癌症和中风患者的血栓前和栓塞病理生理学,特别是在标准评估后中风机制尚未确定的情况下。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#缺血性#
44
#Neurol#
39
#标志物#
32
#缺血性脑#
49
#癌症患者#
48
学习知识
69