EASD2019:重磅!VERIFY研究结果公布:早期联合可显著减少T2DM起始治疗失败相对风险49%
2019-09-22 不详 国际糖尿病
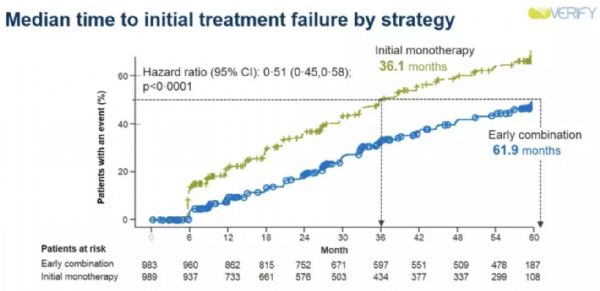
2019年9月18日,一项为期5年、全球多中心、随机、平行对照、双盲临床研究(VERIFY)结果在第55届欧洲糖尿病研究协会(EASD)年会上公布,并同时发表在当天出版的Lancet上。研究结果显示,针对新诊断2型糖尿病(T2DM)患者早期应用维格列汀与二甲双胍联合治疗,比单独应用二甲双胍(目前新诊断T2DM患者治疗标准)能更好地长期控制血糖,降低治疗失败率。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASD#
53
#研究结果#
35
#结果公布#
41
#治疗失败#
47
学习
81
#EASD#
36
#重磅#
34