Eur Arch Otorhinolaryngol:粘膜下鼻甲成形术治疗难治阻塞性鼻炎的疗效如何?
2022-02-25 AlexYang MedSci原创
比较了微型吸绞器辅助的下鼻甲成形术和量子分子共振(QMR),评估了患者的看法和呼吸系统结果。
鼻甲肥大和随之而来的慢性鼻阻塞在普通人群中非常常见,且与过敏性鼻炎和粘膜血管运动亢进等疾病有关。尽管有各种治疗疗法,但慢性阻塞患者往往对局部皮质激素或减充血剂表现出抗拒,症状控制不佳,从而降低了相关的生活质量。

难治性下鼻甲肥大需要用手术方法来治疗。粘膜下方法在恢复呼吸功能和保护鼻粘膜方面具有较好的效果。微型吸绞器辅助下的鼻甲成形术(MAT)能够有效地减少软组织,该手术采用了与射频动能不同的原理。近期,来自意大利的研究人员在《Eur Arch Otorhinolaryngol》上发表文章,比较了微型吸绞器辅助的下鼻甲成形术和量子分子共振(QMR),评估了患者的看法和呼吸系统结果。
研究人员从大学医疗中心前瞻性地招募了因下鼻甲肥大而导致双侧鼻腔持续堵塞的受试者。患者随机分配到每种治疗方法中,并在基线和治疗后30、90和180天,通过视觉模拟评分和内窥镜评估进行症状评估。
结果发现,共有70名参与者完成了评估,其中35人在MAT组,35人在QMR组。这两种方法在使用1个月后,鼻部不适症状均明显减少。MAT组报告的术后出血和水肿比例比QMR组高。在长期随访中,鼻甲大小有类似的明显减少。MAT组在术后第1个月开始报告的VAS结果比QMR组更高。此外,MAT组的手术时间更长,但差异没有统计学显著意义。
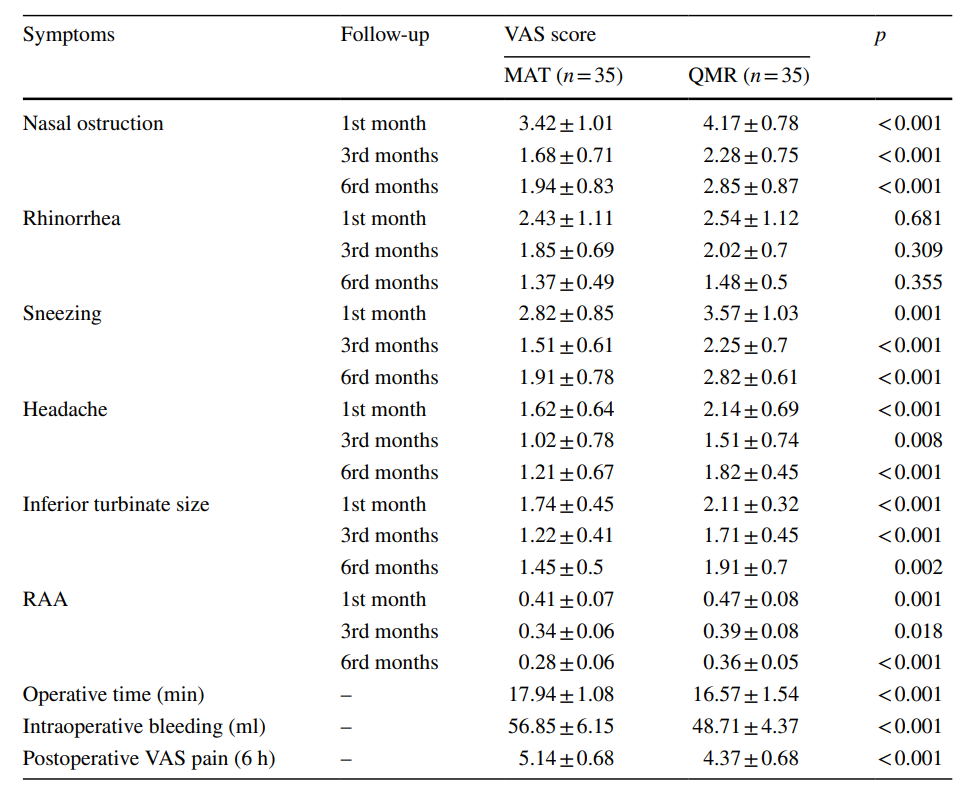
术后手术结果的组间分析
综上所述,MAT通过缩小下鼻甲肥大患者的鼻甲尺寸,可有效控制鼻腔症状。另外,QMR引起的术后并发症较少,其功能效果在长期随访中与MAT相当。
原始出处:
Antonino Maniaci , Jerome Rene Lechien , Ignazio La Mantia et al. Effectiveness of submucosal turbinoplasty in refractory obstructive rhinitis: a prospective comparative trial. Eur Arch Otorhinolaryngol. Jan 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#成形术#
38
#阻塞#
39
#粘膜#
44
请问OMR是什么?哪位大神来解释一下
36
很好
46
不错学习了。
54