双膦酸盐相关性颌骨坏死并发腕部舟状骨骨髓炎1例
2020-04-03 孙照薇 李志勇 余丹 华西口腔医学杂志
双膦酸盐类药物是一种治疗骨质疏松及防治癌症全身骨转移的临床常用药,使用时间已超过15年,临床使用患者数量众多,且多为长期规律用药。2003年Mark首次报道了双膦酸盐类药物相关性颌骨坏死(bispho
双膦酸盐类药物是一种治疗骨质疏松及防治癌症全身骨转移的临床常用药,使用时间已超过15年,临床使用患者数量众多,且多为长期规律用药。2003年Mark首次报道了双膦酸盐类药物相关性颌骨坏死(bisphosphonate-related osteonecrosis of the jaw,BRONJ),自此双膦酸盐类药物在骨坏死发生方面的副作用被广泛关注。
BRONJ在用药人群中的发病率可达到18.6%,根据用药方式与具体药物的不同,发病率可有明显差异。静脉使用发病率明显高于口服用药,含氮双膦酸盐使用发病率明显高于不含氮双膦酸盐,唑来膦酸静脉注射后发病率最高。虽然BRONJ临床常见,已引起了临床相关科室的关注,但相关病例报告及讨论在国内报道较少。药物相关性骨坏死多发生于颌骨,这可能是由于颌骨改建活跃,血供较少,更容易形成死骨。本文报道1例双膦酸盐相关性颌骨坏死并发腕部舟状骨骨髓炎。
1.病例报告
患者男性,30岁,2017年5月门诊主诉“右下颌拔牙创不愈伴反复肿痛3年”收入院。现病史:2015年9月拔除48阻生牙(图1),术后拔牙创长期未愈,右下后牙区牙龈反复肿胀疼痛。2016年3月拔牙术后复诊CT显示右下颌骨磨牙区形成死骨块,边界清晰,46根尖处牙槽骨吸收(图2)。2016年5月主诉“右下拔牙创不愈伴反复肿痛2年”来院就诊。近来患者自觉右下后牙区骨质暴露,影响咬合。门诊诊断为“药物相关性颌骨坏死”。
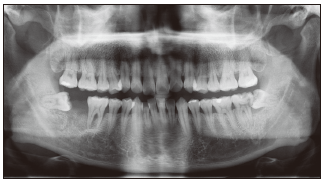
图1 拔牙术前全景片(2015.9)示48近中阻生

图2 下颌骨CT(2016.3)可见右下颌磨牙区死骨边界清晰,46根尖处牙槽骨吸收
既往史:2012年患者确诊非小细胞肺癌,间变性淋巴瘤激酶(anaplastic lymphoma kinase,ALK)(+),乙肝表面抗原(HB-SAg)(+),e抗体(HBeAb/抗-HBe)(+)。化疗1年未见好转,现服用克唑替尼靶向治疗,口服,每日2次。未进行过放疗,病情控制尚可。2013年3月开始规律静脉注射唑来膦酸防止全身骨转移。连续用药26个月后至2015年5月停用唑来膦酸。2016年10月主诉腕部红肿痛伴活动受限5月余,加重2月余,剧烈活动后左腕部明显肿胀伴剧烈疼痛,双手腕部均未受过外伤。取活组织检查切口见白色脓液渗出,切口持续不愈。
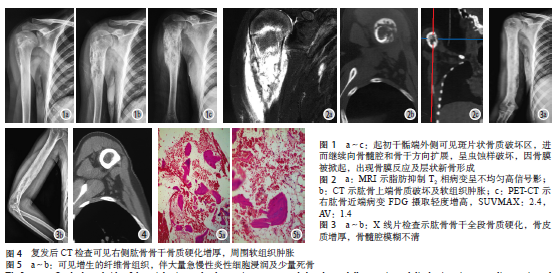
腕部MRI显示左腕部骨水肿改变,舟状骨囊性退变,关节腔积液。腕部X线平片显示舟状骨中心低密度区,骨质破坏吸收(图3)。于本院手外科施慢性溃疡修复术,术后常规使用抗生素。术后病理显示腕部舟状骨软组织慢性化脓性炎症伴局部肉芽肿炎,纤维组织增生,死骨片及软骨变性,细菌培养阴性,未见恶性肿瘤证据(图4)。诊断为腕部舟状骨中心性骨髓炎,未明确病因。

图3 左腕部X线平片(2016.10)见舟状骨中心低密度区
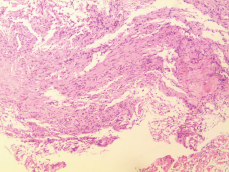
图4 术后病理报告(2016.10)显示软组织大量肉芽组织伴纤维组织增生,可见死骨片及软骨变性,未见放线菌感染
检查:患者面形不对称,右面部略肿胀,骨质膨隆,无压痛,前牙开,46牙松动度2度,远中见一黄白色死骨暴露,龈瓣增生覆盖,口内腐臭味明显,全口牙龈无明显红肿(图5)。全景片及CBCT显示46牙远中骨质破坏影,密度不均,死骨形成,边界较清,46牙槽骨破坏至根尖,其他牙位未见明显牙槽骨吸收(图6)。左腕部可见术后瘢痕(图7)。

图5 术前口腔检查(2017.5)见患者口内右下颌磨牙区死骨形成,龈瓣增生覆盖

图6 术前全景片(2017.5)可见死骨块边缘清晰,46牙槽骨破坏至根尖

图7 左腕部可见术后瘢痕(2017.5)
入院诊断:双膦酸盐相关性颌骨坏死。治疗:行右下颌骨部分切除术+口腔颌面部软组织缺损局部组织瓣修复术+周围神经嵌压松解术。术中拔除46牙,去除后牙区死骨块,刮除腔内炎性肉芽组织,碘仿纱条填塞,术后常规使用抗生素。术后病理显示右下颌骨软组织炎性肉芽肿组织伴坏死,较多死骨组织伴钙化及大量放线菌团样物,未见恶性肿瘤证据(图8)。
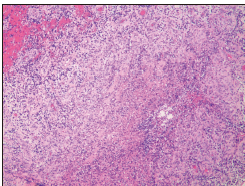
图8 术后病理(2017.5)显示软组织大量肉芽组织伴坏死,可见钙化及放线菌团样物
复诊:术后3个月复诊,肉眼观察可见手术创口愈合良好,软组织形态正常,面形对称无明显膨隆,余留牙形态正常,牙龈未见红肿(图9)。全景片、CT显示右侧手术创骨皮质增厚,可见新骨形成,未见新发死骨及骨髓炎(图10、图11)。

图9 手术创口愈合良好,软组织形态正常(2017.8)
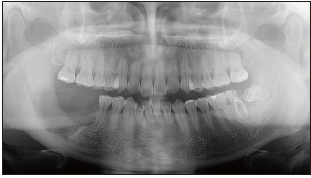
图10 全景片(2017.8)可见原死骨处已形成光滑连续骨皮质,未见新生死骨
图11 CT(2017.8)可见右下颌磨牙后区形成边界光滑清晰骨皮质,未见新生死骨
2.讨论
双膦酸盐类相关颌骨坏死的病因主要为以下几个方面。
1)双膦酸盐类药物直接作用于破骨细胞,抑制破骨细胞功能与活性,旧骨吸收减少,使骨改建倾向于成骨方向,局部出现骨密度增加、骨硬化,破坏骨稳态。双膦酸盐进入人体后可在骨中沉积十几年甚至数十年无法彻底代谢,这使得双膦酸盐对破骨细胞的抑制作用也可以持续十几年。因此在使用双膦酸盐类后,相关颌骨坏死可发生于十几年后。由于颌骨是成人骨改建最活跃的部分,因此BRONJ多发生于颌骨。双膦酸盐类药物对骨稳态的影响是颌骨坏死发生的主要原因之一。
2)双膦酸盐类药物作用于血管,抑制血管内皮细胞迁移与黏附,抑制小血管及微血管的生成,使形成的新骨中血管含量降低,造成局部缺血缺氧环境。唑来膦酸对血管生成的抑制作用已经在体外细胞实验层面得到证实。
3)双膦酸盐相关颌骨坏死常发生于使用双膦酸盐类药物的患者颌骨发生创伤之后,常见拔牙等原因。拔牙后拔牙创长期无法愈合导致死骨更易形成,有研究者认为双膦酸盐类药物有一定的软组织毒性可能是软组织无法愈合的原因之一。体外实验中也证实,双膦酸盐类药物可以影响纤维细胞的形成与功能,唑来膦酸可以明显抑制口腔上皮细胞的增殖。
4)由于患者拔牙后创口长期难以愈合,创口开放导致细菌感染发生。BRONJ患者死骨及拔牙创病理检查常发现大量放线菌存在。因此细菌感染是死骨形成、BRONJ发生的病因之一。
5)某些基因多态性可能是BRONJ个体易患因素。本文病例肺癌4年规律靶向药治疗,未进行过放疗,同时规律静脉注射唑来膦酸27个月,停药后4个月拔除48阻生齿,拔牙创长期未愈合,拔牙后半年拔牙创可见死骨形成,手术去除死骨后,病理显示肉芽组织伴钙化和死骨,同时存在放线菌团,符合既往研究中关于BRONJ病因的猜测。但该患者较为特殊的一点在于,药物相关性骨坏死常见于颌骨,尤其是骨改建活跃、血供较少的下颌骨,而该患者骨髓炎症状同时发现于左手腕部舟状骨,腕部CT显示,患者左手舟状骨有中心性骨坏死灶。
流行病学证据表明,躯干骨骨髓炎病因多为外伤、血源性感染、免疫抑制等。病史显示患者双手腕部均未受过外伤,未使用免疫抑制剂,无血液疾病,无感染性疾病。腕部无菌性骨坏死及舟状骨骨折后长期不愈者的病因与腕部骨解剖结构有关。腕部舟状骨呈腰细头尾粗的形态,80%表面覆盖有软骨,远端由桡动脉供血,近端仅有桡舟月韧带带来极少供血。
由于舟骨的解剖特征,在腕部受到外力作用后容易造成骨折及骨结构的微损伤,且伤后较难愈合。结合该患者病史,可排除上述较常见的骨髓炎病因。考虑到其唑来膦酸静脉注射用药史及颌骨坏死的临床表现,笔者认为该患者腕部舟状骨坏死可能与双膦酸盐用药史相关。双膦酸盐可能影响患者血管的生成,导致微血管改变和减少,造成舟状骨腰部缺血性坏死。
另一方面,双膦酸盐的使用抑制了破骨细胞的作用,使骨皮质增厚,骨密度增大,在一定程度上降低了骨的应力作用。由于骨缓冲能力降低,骨皮质微创伤增加,不断积累,造成骨的微小改变。
综上,该患者最终形成了腕部舟状骨的无菌性中心性坏死。病理证实患者左侧腕部舟状骨未发现放线菌存在,细菌培养阴性。除细菌阴性外,其余病理特征与颌骨死骨病理改变相同(大量肉芽组织伴钙化团,可见骨片与死骨形成)。因此,高度怀疑该患者双侧腕部舟状骨骨髓炎与右下颌颌骨骨髓炎同样具有唑来膦酸相关性。目前对双膦酸盐类颌骨坏死并无十分有效的治疗方法,多采用对症治疗。
早期采用抗菌药局部冲洗,控制炎症,全身系统使用抗生素,亦有使用特里帕肽和高压氧治疗。部分患者形成死骨后考虑采用手术方法去除已有死骨,但无法改善骨密度增加症状,多年甚至数月后仍可能复发形成死骨。且手术本身带来创伤,可能加重感染或创口。
因此术前要严格控制适应证并加强围手术期管理:1)通过影像学确定死骨范围,尽量减少手术创伤;2)彻底清除受累骨质,减少复发可能;3)去除死骨后彻底清除术腔内肉芽组织和尖锐骨缘骨刺,减少刺激;4)术后病灶使用健康软组织做无张力覆盖封闭;5)术后使用抗生素,预防感染,至软组织愈合;6)创口完全愈合前不使用义齿假体等修复。
本例患者死骨已游离,范围明确清晰,无红肿,软组织充足,坏死少,因此采用手术去除死骨,刮除腔内肉芽组织,术后配合使用抗生素,促进创口愈合。双膦酸盐代谢较慢,在骨内可沉积多年,因此对于拟长期使用双膦酸盐(尤其是唑来膦酸静脉注射)的患者,用药前应注意进行全面口腔检查,拔除阻生齿,去除口内不良修复体,保持牙周状况良好等。长期用药过程中要定期检查全身骨状况,预防及控制骨坏死的发生发展。
原始出处:
孙照薇,李志勇,余丹,朱洁颖,张伊殿,朱鑫美.双膦酸盐相关性颌骨坏死并发腕部舟状骨骨髓炎1例[J].华西口腔医学杂志,2019(02):224-228.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#相关性#
31
#骨坏死#
43
#并发#
25
#坏死#
33
#骨髓炎#
36
#颌骨坏死#
29