指导肿瘤切除的新利器:纳米荧光传感器
2016-12-24 佚名 生物谷
—根据一项最新研究,一种新型纳米荧光传感器可以特异性地在肿瘤组织“打开”并发出荧光,帮助医生准确切除肿瘤组织,并在最大程度上保留正常组织,这项研究成果发表在《自然—生物医学工程》杂志上。 据研究人员报道,这项突破性的技术适用于任何类型的肿瘤,他们将在明年进行人体临床试验。 据报道,研究人员将这种纳米探针注射到小鼠的肿瘤组织后,一旦接触肿瘤细胞,这种探针就会打开并照亮肿瘤组织。 “这表明
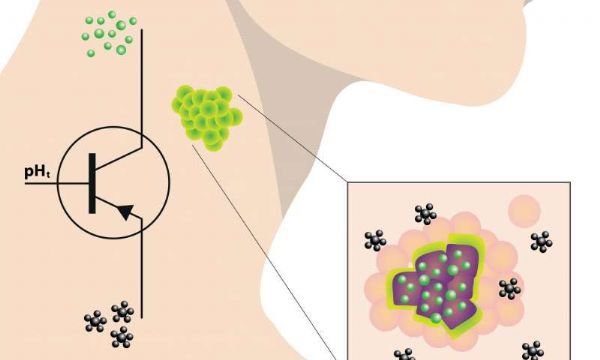
—根据一项最新研究,一种新型纳米荧光传感器可以特异性地在肿瘤组织“打开”并发出荧光,帮助医生准确切除肿瘤组织,并在最大程度上保留正常组织,这项研究成果发表在《自然—生物医学工程》杂志上。
据研究人员报道,这项突破性的技术适用于任何类型的肿瘤,他们将在明年进行人体临床试验。
据报道,研究人员将这种纳米探针注射到小鼠的肿瘤组织后,一旦接触肿瘤细胞,这种探针就会打开并照亮肿瘤组织。
“这表明与正常组织相比,人肿瘤组织偏酸性,我们也正是利用了肿瘤组织的这个特点。”论文共同作者Baran Sumer说,他是德克萨斯大学西南医学中心的一名外科医生。
对许多肿瘤而言,手术是首选治疗方案。但是要完全清除肿瘤组织并尽可能保留正常组织在目前仍然是一个巨大的挑战,因为目前的影像技术不够灵敏,无法准确区分肿瘤组织与非肿瘤组织。
而这项新技术使用了临床批准的荧光染料,可以通过全世界医院正在使用的标准照相机进行成像。这种纳米探针就像传感器一样,只有所处环境的pH值低于阈值时,它才会打开并发出荧光。
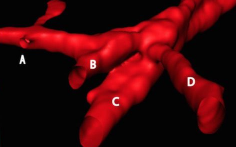
研究人员在小鼠头颈癌模型中进行了实验,他们发现在手术中使用这种探针具有极强的特异性和敏感性,它甚至可以照亮直径小于1 mm的肿瘤结节。
“进行手术时,这种探针可以为外科医生准确描绘出肿瘤边界。”Sumer说道。
这是一种纳米尺度的开关技术,迄今为止还没有任何一项技术具有这么高的精确度。
“制备这种探针相对简单,因此成本也不高,”Sumer解释道。“我坚信这项技术可以用于人体内肿瘤边界的检测。”
原始出处
Tian Zhao et al. A transistor-like pH nanoprobe for tumour detection and image-guided surgery, Nature Biomedical Engineering (2016).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#荧光#
34
#肿瘤切除#
46
#荧光传感器#
0
#传感器#
28