CELL:中科院杨辉团队利用CRISPR系统,实现胶质细胞向神经元转化
2020-04-09 MedSci原创 MedSci原创
神经胶质细胞转化为功能性神经元代表了一种潜在的治疗方法,用于补充与神经退行性疾病和脑损伤相关的神经元损失。
神经胶质细胞转化为功能性神经元代表了一种潜在的治疗方法,用于补充与神经退行性疾病和脑损伤相关的神经元损失。
以前在这方面的尝试,包括过表达转录因子在体内产生所需的神经元类型导致的低转换效率和失败,阻碍了这一领域的尝试。
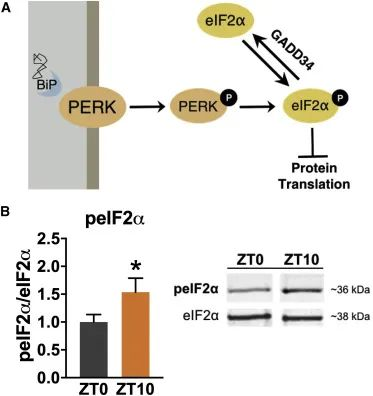
最近,研究人员报告说,使用最近开发的RNA靶向CRISPR系统CasRx的体内病毒递送,下调一个单一的RNA结合蛋白,多嘧啶束结合蛋白1(Ptbp1),能够导致Müller胶质体转化为视网膜神经节细胞(RGCs),并且转换效率很高,导致与RGC损失相关的疾病症状的缓解。
此外,这种方法还诱导了纹状体中具有多巴胺能特征的神经元,缓解了帕金森病小鼠模型的运动缺陷。
因此,由CasRx介导的Ptbp1敲除的胶质体到神经元的转换代表了一种有前途的体内遗传方法,可以用于治疗各种神经元缺失引起的疾病。
原始出处:
Haibo Zhou et al. Glia-to-Neuron Conversion by CRISPR-CasRx Alleviates Symptoms of Neurological Disease in Mice. CELL (2020). DOI:https://doi.org/10.1016/j.cell.2020.03.024
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#中科院#
48
#Cell#
50
#CEL#
45
#CRISPR#
33
#胶质细胞#
32