胃癌晚期,不能手术“等死”?医生这样救了她
2018-04-20 李东/上海交通大学医学院附属瑞金医院 澎湃新闻
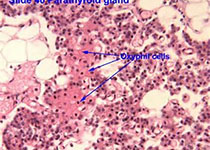
今天是42岁的赵春梅出院的日子,几个月前因查出胃癌而被宣告不治的她,在瑞金专家的精准方案下明显好转,此刻正高兴地指挥着丈夫老陈上下收拾回家的行囊。几年前,赵春梅(化名)发现自己饭后总是胃胀、反酸。慢慢的,她开始吃不下饭了,人暴瘦了10多斤。上腹严重的胀痛让一向自诩身强体壮的她扛不住了,去年十一在海门当地做了个胃镜。“胃黏膜增厚”,看到这五个字时,丈夫老陈的心上咯噔一声,意识到这或许不是个好兆
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好知识值得拥有
63
学习了
55
晚期癌症.提高生活质量为主.缓解病人痛苦为主
63
学习了.谢谢
50
学习了
55
最后一段非常好 学习了
26
学习了很有用
21