BMJ:巨大胸甲状腺肿所致的呼吸困难
2016-09-28 MedSci MedSci原创
女性患者,80岁,因劳累时呼吸困难,并伴有嘈杂呼吸音而就诊于急诊科。患者可完整说话表达思想,但是体格检查发现有微弱的双相喘鸣。患者自述症状已有数月,且逐渐恶化。患者无复调的呼气性喘鸣音。其他健康状况良好。胸片如下所示(图1⇓)。胸片显示大的纵隔肿块,气管明显偏右侧(图2,T⇓)。对于这样一个肿块的鉴别诊断包括畸胎瘤、胸腺增大、淋巴结肿大和胸骨后甲状腺肿大。鉴于患者症状的长期性和病情的稳定性,因此没
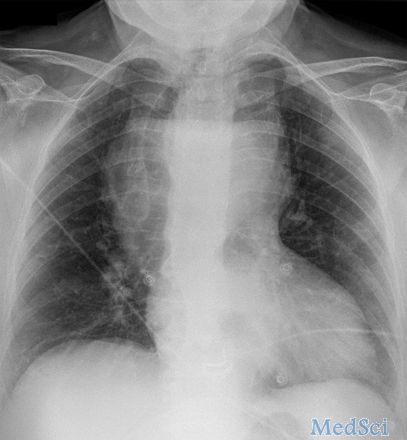
女性患者,80岁,因劳累时呼吸困难,并伴有嘈杂呼吸音而就诊于急诊科。患者可完整说话表达思想,但是体格检查发现有微弱的双相喘鸣。患者自述症状已有数月,且逐渐恶化。患者无复调的呼气性喘鸣音。其他健康状况良好。胸片如下所示(图1⇓)。
胸片显示大的纵隔肿块,气管明显偏右侧(图2,T⇓)。
对于这样一个肿块的鉴别诊断包括畸胎瘤、胸腺增大、淋巴结肿大和胸骨后甲状腺肿大。鉴于患者症状的长期性和病情的稳定性,因此没必要立刻考虑其气道通气问题。但是仍立即进行了CT扫描(图3⇓)。肿块的边缘(M)可追踪到锁骨以上,因此最可能的诊断是甲状腺肿大。
CT扫描可以追踪肿块的边缘(M),并显示与甲状腺左叶相连(C)。甲状腺叶也可显示(T)。肿块体积较大,最初是从前纵隔进入胸腔。这是常见的胸内甲状腺肿。然而,随着肿块下移,后移进入中纵隔,从而造成气管向右侧移位。
原始出处:
Joseph Dalby Sinnott, David C Howlett. Dyspnoea in an older woman. BMJ 2016; 354 doi: http://dx.doi.org/10.1136/bmj.i4883.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
25
#甲状腺肿#
30
#呼吸困难#
32