血清铁蛋白可提高前列腺癌诊治准确性
2017-02-23 冯亮 中华医学信息导报
近日,浙江大学研究人员通过对近3000例前列腺癌患者的对照研究,发现血清铁蛋白可提高前列腺癌预测的准确性,在前列腺癌诊断与预后判断中具有重要应用价值。相关论文于2月2日在线发表在国际学术期刊《肿瘤靶标》。
近日,浙江大学研究人员通过对近3000例前列腺癌患者的对照研究,发现血清铁蛋白可提高前列腺癌预测的准确性,在前列腺癌诊断与预后判断中具有重要应用价值。相关论文于2月2日在线发表在国际学术期刊《肿瘤靶标》。
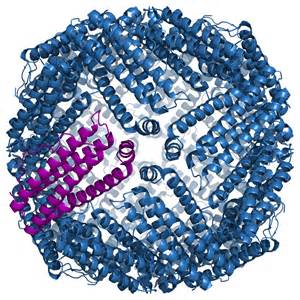
“此前的研究中,多种肿瘤患者的血清铁蛋白水平存在升高现象,提示血清铁蛋白可能是恶性肿瘤潜在的生物标记物。”论文通讯作者之一、浙江大学公共卫生学院王福俤教授介绍:“铁蛋白是人体内存储铁的主要蛋白,近年来的研究发现血清铁蛋白的升高与免疫抑制、血管生成和增殖等一系列病理过程有关。”
研究人员对2002例前列腺癌患者及951例前列腺增生患者的临床数据进行收集和分析,发现血清铁蛋白升高使前列腺癌患病风险显着增加。而随着前列腺癌恶性程度增加,人体内组织铁蛋白和血清铁蛋白也均升高,两者具有高度相关性。研究人员表示,该成果表明血清铁蛋白可作为辅助诊断的无创生物标记物用于前列腺癌的诊断与预后评估。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#血清铁#
36
#准确性#
31
#血清铁蛋白#
0