NEJM:小儿胱氨酸病-案例报道
2015-12-03 chenshuo译 MedSci原创
女性,1岁,伴有生长发育障碍、轻度贫血、低磷血症、维生素D缺乏、糖尿、蛋白尿等到院就诊。
女性,1岁,伴有生长发育障碍、轻度贫血、低磷血症、维生素D缺乏、糖尿、蛋白尿等到院就诊。

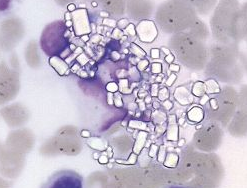
接受骨髓穿刺检查,发现骨髓内存在多边形胱氨酸晶体且巨噬细胞比例升高(20%;正常范围值为2-5%),最后会诊医师确诊该女童患上了小儿胱氨酸病。
小儿胱氨酸病一种罕见的常染色体隐性遗传病,因胱氨酸晶体贮积在溶酶体内而导致病变。游离胱氨酸可累积在细胞溶酶体内,包括肝细胞、肾脏、眼睛和大脑等。
对于小儿胱氨酸病的诊断,一般是通过光镜下观察胱氨酸晶体是否存在或通过测量白细胞内胱氨酸的含量来判断。
虽然胱氨酸晶体在裂隙灯检查或骨髓诊断可以观察到,但年龄小于1岁的患儿体内通常难以发现胱氨酸晶体的存在,这给临床诊断带来了很大的难题。
随后,该女童接受了应用半胱胺药物进行治疗,临床症状也有所好转。
不幸的是,8个月后,该女童在住院期间因全身感染而死亡。
原始出处:
Perla Vicari, M.D., Ph.D.and Vivia M. Sthel, M.D., Ph.D.Cystine Crystals in Bone Marrow,N Engl J Med 2015
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








谢谢分享。
97
遗传代谢,不可漏诊
53
这篇文章有一定深度
110
是一篇不错的文章
49
值得进一步关注
68
不错,赞一个
100
好文章,值得收藏
96
个案
86