JAMA Neuro:Aβ水平的空间范围以及与Tau-PET和认知的相关性研究
2022-08-31 MedSci原创 MedSci原创
区域性Aβ结合似乎在生物学上是相关的,在这个阶段的参与者仍然相对没有CSF磷酸化的tau181、tau-PET结合和相关的认知衰退,使他们成为抗淀粉样蛋白药物的理想目标。
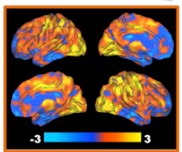
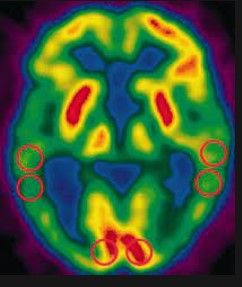
抗淀粉样蛋白制剂的预防试验最好招募在正电子发射断层扫描(PET)上最早显示出生物相关β-淀粉样蛋白(Aβ)结合的人。近期发表在JAMA Neurology杂志上的研究探讨了Aβ-PET结合开始显示与阿尔茨海默病(AD)的其他标志物相关的时间。
这项纵向的多中心队列研究包括3个独立的队列:PREVENT-AD(数据收集于2012-2020年),ADNI(2005-2019年),以及HABS(2011-2019年)。在Aβ-PET结合空间范围的3级分类中,如果个人在指定的一组容易出现早期Aβ积累的脑区中显示阳性信号,则被指定为具有广泛的Aβ沉积。那些在部分但不是全部有结合的人被归类为有区域性沉积。所有在第一次Aβ PET扫描时认知能力无障碍的参与者。主要结果是脑脊液(CSF)的差异、遗传学、tau-PET负担和认知能力下降。
结果共纳入817名参与者,包括129名来自PREVENT-AD队列(平均[SD]年龄,63.5[4.7]岁),400名来自ADNI(平均[SD]年龄,73. 6[5.8]岁),以及288名来自HABS(平均[SD]年龄,73.7[6.2]岁)。与Aβ阴性者相比,那些有区域性Aβ结合的人显示出更多的APOE ε4携带者(18 [64%] vs 22 [27%] PREVENT-AD和34 [31%] vs 38 [19%] ADNI),CSF Aβ1-42水平降低(F = 24和71),以及更大的纵向Aβ-PET积累(显著β = 0.019)。

广泛的淀粉样蛋白结合的参与者进一步表现出明显的认知下降(显着β=-0.014至-0.08),更大的CSF磷酸化tau181(F = 5和27),和tau-PET结合(所有F > 7.55)。使用每个队列规定的Aβ阳性的二分法阈值或视觉阅读分类,大多数参与者(56%至100%,取决于分类方法和队列)的区域Aβ会被归类为Aβ阴性。
综上,区域性Aβ结合似乎在生物学上是相关的,在这个阶段的参与者仍然相对没有CSF磷酸化的tau181、tau-PET结合和相关的认知衰退,使他们成为抗淀粉样蛋白药物的理想目标。
参考文献:
Spatial Extent of Amyloid-β Levels and Associations With Tau-PET and Cognition.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
44
#相关性#
35
#PET#
65
#Tau#
57
#Aβ#
65
JAMA上文章都是顶级的,谢谢梅斯及时上新
0