European Radiology:MRI扩散特征指数,实现浸润性乳腺癌组织学表型的无创评估!
2022-08-18 shaosai MedSci原创
雌激素受体(ER)、孕激素受体(PR)、人表皮生长因子受体2(HER2)和增殖状态(Ki-67)的表达程度是指导侵袭性乳腺癌治疗决策的主要预后因素。
现阶段,扩散加权成像(DWI)已被广泛应用于诊断和监测许多器官的肿瘤性病变。为了量化组织的扩散性,通常要计算表观扩散系数(ADC),并由此生成ADC图。在乳腺病变中,在常规动态对比增强(DCE)MRI中加入DWI序列对乳腺癌的检测和诊断、治疗反应监测和预后预测方面都表现出极大的价值。
雌激素受体(ER)、孕激素受体(PR)、人表皮生长因子受体2(HER2)和增殖状态(Ki-67)的表达程度是指导侵袭性乳腺癌治疗决策的主要预后因素。这些标志物一般从活检样本中获得,但高达20%的患者在活检和手术标本之间可能出现受体或增殖状态的差异。因此,有必要使用术前非侵入性标志物来预测组织学状态。
最近有研究提出了更先进的DWI模型用于乳腺DWI的诊断,特别是对非高斯扩散(高扩散加权)和血液微循环(体内非相干运动[IVIM],低扩散加权)敏感的模型。IVIM/非高斯扩散模型提供了有关组织微循环和微结构的宝贵信息,并有可能提供额外的信息来描述标准ADC以外的病理或生理肿瘤状况。然而,这些模型需要在很大的b值范围内采集多个信号,导致采集时间长和高级后处理,这两个部分通常与正常的临床使用不兼容。
签名指数(S-index)为一种先进的DWI标志物,其整合了IVIM和非高斯扩散信息且不需要建模。S-指数反映了典型的良性和恶性组织信号库之间的扩散信号衰减的相似性,以及使用一组仅有的两个关键b值。有研究发现,S-指数和DCE MRI在区分乳腺恶性病变和良性病变方面具有同等的诊断性能,并提高了DCE MRI对病变诊断的特异性。此外,S-指数在浸润性乳腺癌中显示出基于PR和HER2表达的不同趋势。
近日,发表在European Radiology杂志的一项研究进一步评估了S-指数与浸润性乳腺癌重要预后因素和分子表型之间的关系,为术前无创的评估浸润性乳腺癌的病理分型及风险分层提供了支持。
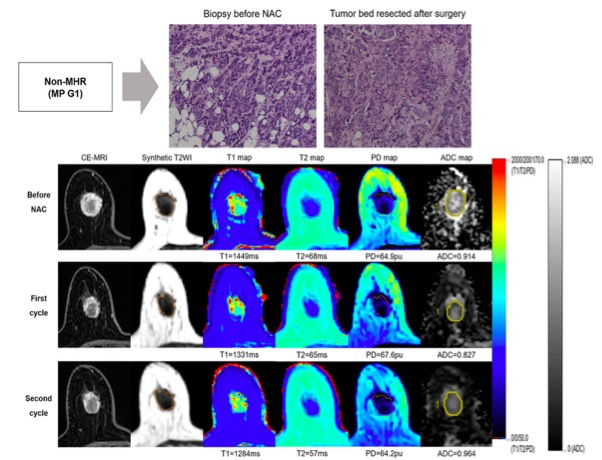
本研究于2017年-2021年期间对浸润性癌患者进行了一项回顾性研究。所有患者都使用3-T系统进行了动态对比增强MRI和DWI。对于DWI,使用三个b值(0、200和1500s/mm2)计算S-指数。在DWI上,在整个肿瘤上手动放置三维ROI。将平均和第85百分位的S指数值与IHC状态、增殖率和病变的分子亚型进行比较。
该研究纳入了153名患者(平均年龄,60±13岁),共160个浸润性乳腺癌病灶。雌激素受体阳性(平均,p = .005;第85百分位数,p < .001)和孕激素受体阳性(平均,p = .003;第85百分位数,p < .001)肿瘤的S指数值明显较高,而人表皮生长因子受体2(HER2)-阳性肿瘤的S指数值明显较低(平均,p = 023;第85百分位数,p < .001)。平均和第85百分位数的S-指数值在乳腺癌亚型中明显不同(平均,p = .015;第85百分位数,p = .002),这些值对预测IHC状态的AUC对HER2分别为0.64和0.66,对激素受体为0.70和0.74。
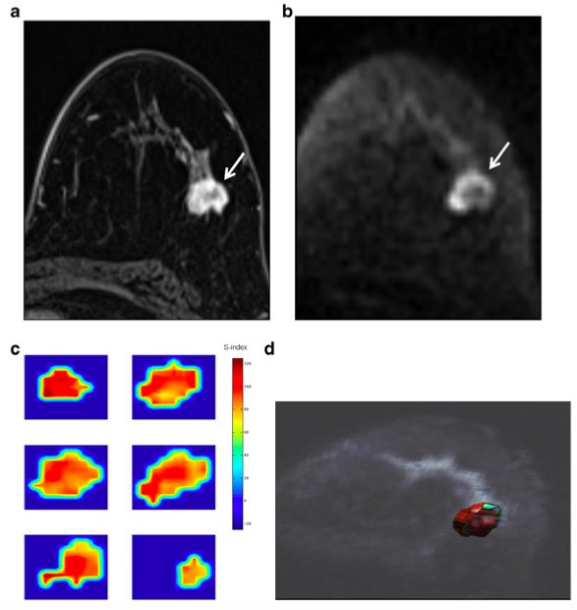
图 50岁女性,患有腺泡A型浸润性导管癌。轴位早期动态对比增强MRI显示左乳有一边缘不规则的肿块(a,箭头)。弥散加权图像(b=1500)清楚地显示了具有高信号强度的肿块(b,箭头)。生成的每个层面(c)和整个肿瘤的三维渲染图(d)的平均特征指数(S-index)图是在感兴趣区层面和逐个体素计算的,显示出了高S-指数(红色)。这个肿块的平均S-指数为90.4,第85百分位数为105
本研究表明,定量弥散MRI的S-指数值与浸润性乳腺癌的预后因素显示出高度的相关性,平均和第85百分位的S-指数值可用于预测HER2和激素受体状态。本研究显示,S-指数是一种简单且便于获得的影像学方法,可以以非侵入性的方式评估浸润性乳腺癌的组织学表型。
原文出处:
Mariko Goto,Denis Le Bihan,Koji Sakai,et al.The diffusion MRI signature index is highly correlated with immunohistochemical status and molecular subtype of invasive breast carcinoma.DOI:10.1007/s00330-022-08562-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
25
#组织学#
52
#浸润性乳腺癌#
35
#表型#
38