J Hepatol:丙酮酸脱氢酶复合物和乳酸脱氢酶是治疗急性肝衰竭的靶点
2018-03-31 MedSci MedSci原创
PDHC和LDH转移到细胞核,是治疗急性肝衰竭的靶点。
研究背景:急性肝衰竭是肝功能迅速恶化,导致高死亡率和高发病率。代谢酶可以在细胞核中转移,以调节组蛋白乙酰化和基因表达。
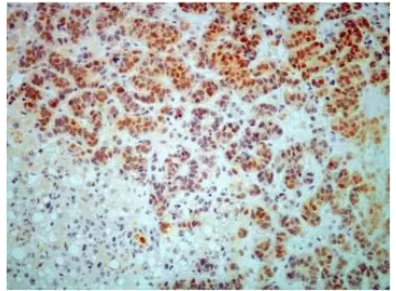
研究方法:在暴露于各种肝脏毒物(CD95-Ab、α-毒蕈环肽、对乙酰氨基酚)的小鼠肝组织的细胞核中评价丙酮酸脱氢酶复合物(PDHC)和乳酸脱氢酶(LDH)的水平和活性。采用RNA-seq对急性肝功能衰竭小鼠的全基因组基因表达谱进行检测,并进行基因本体富集分析。在暴露于各种肝脏毒物的小鼠中,评价组蛋白乙酰转移酶抑制剂-garcinol和LDH抑制剂-galloflavin在减轻肝损伤上面的疗效。
研究结果:在急性肝功能衰竭的小鼠的肝细胞浆体和细胞核中,PDHC和LDH的水平和活动均增加。细胞核PDHC和LDH的增加与细胞核中乙酰辅酶A和乳酸的浓度增加和组蛋白H3超乙酰化有关。急性肝功能衰竭小鼠肝脏的基因表达提示,组蛋白H3乙酰化的增加诱导了对损伤的反应的基因的表达。组蛋白乙酰转移酶抑制剂-garcinol降低组蛋白乙酰化,降低肝损伤,改善急性肝衰竭小鼠的生存。暴露于促凋亡刺激的细胞中,PDHC或LDH的敲除,提高了细胞生存能力。在急性肝功能衰竭的小鼠中,LDH抑制剂-galloflavin被发现抑制了PDHC的活性、减轻了肝坏死、凋亡和促炎细胞因子表达。
研究结论:PDHC和LDH转移到细胞核,是治疗急性肝衰竭的靶点。
原始出处
Ferriero R, Nusco E, De Cegli R, et al. Pyruvate dehydrogenase complex and lactate dehydrogenase as targets for therapy of acute liver failure. J Hepatol, 2018 Mar 23. doi: 10.1016/j.jhep.2018.03.016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肝衰#
27
#复合物#
37
#急性肝衰竭#
36
#EPA#
26
学习了.有用
63
厉害了我的哥
53