Nat Med:CAR脱轨!CAR-T治疗意外搞出“CAR-癌细胞”,宾大科学家发现CAR-T治疗后复发的罕见机制
2018-10-07 奇点糕 奇点网
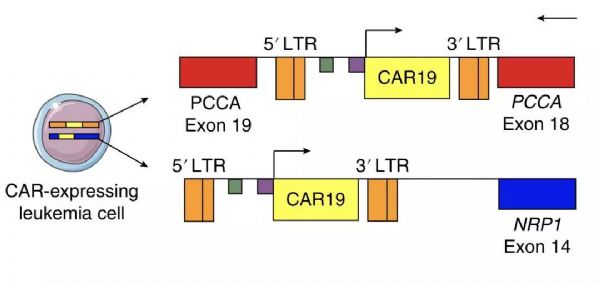
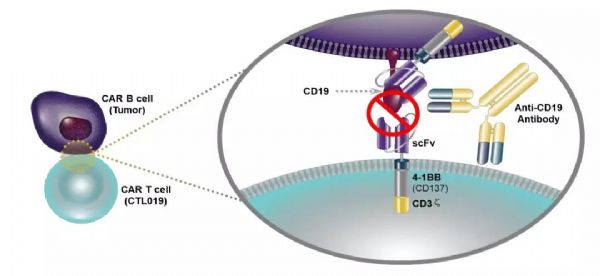
在给一名身患复发/难治性B细胞急性淋巴细胞白血病(B-ALL)的患者生产CAR-T细胞时,那个本该加到T细胞上,帮助T细胞特异性识别CD19、并抓住癌细胞的CAR(嵌合抗原受体),意外地被加到患者癌变的B细胞上,形成了“CAR-癌细胞”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
23
#科学家发现#
26
#CAR-#
26
#癌细胞#
30
#罕见#
32
#Med#
17
学习了谢谢
70