病例分享:吲哚布芬用于房颤卒中合并消化道出血患者抗栓治疗1例
2019-03-27 耿小勇 中华医学信息导报
复杂缺血性心肌病患者PCI术后消化道出血,并伴发房颤、脑栓塞,依据缺血/出血风险评估量表动态调整抗栓方案。应用吲哚布芬+OAC方案短期应用安全过渡后单用吲哚布芬抗栓治疗。兼顾抗血小板、抗凝治疗适应症,患者随访至今未发生缺血/出血并发症。
病例特点介绍
复杂缺血性心肌病患者PCI术后消化道出血,并伴发房颤、脑栓塞,依据缺血/出血风险评估量表动态调整抗栓方案。应用吲哚布芬+OAC方案短期应用安全过渡后单用吲哚布芬抗栓治疗。兼顾抗血小板、抗凝治疗适应症,患者随访至今未发生缺血/出血并发症。
病史资料
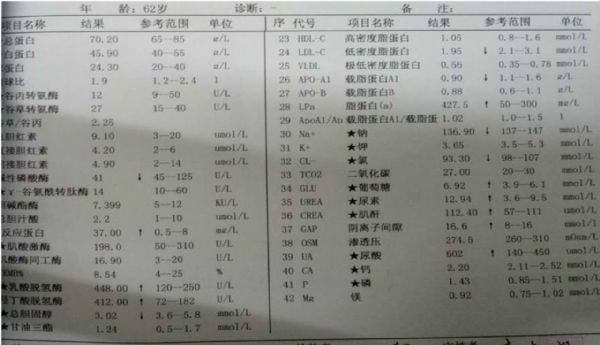
患者:男性,62岁,85 kg。
就诊时间: 2017年5月16日(第一次入院)。
患者主诉:主因间断胸闷3年,加重伴心悸、喘憋3天入院。
现病史:3年来活动后出现胸闷,持续数分钟至十余分钟不等,未予正规诊治,今日上述症状发作频繁,3天来加重,休息中亦有发作伴心悸喘憋,休息或含服硝酸甘油后稍好转,持续半小时至数小时。
危险因素:高血压病史20余年,最高180/100 mmHg,间断服药治疗,平素血压波动于150/90 mmHg左右;吸烟史40年,2型糖尿病20余年,未正规用药及监测血糖。
体格检查:神清语利,BP 155/95 mmHg,双肺呼吸音稍低,双下肺可闻及湿罗音,心界左侧扩大,HR 90次/分左右,心律齐,心音低钝,双下肢轻度指凹性水肿。
初步诊断:冠状动脉粥样硬化性心脏病、急性冠脉综合征、Killip Ⅱ级;高血压病3级 ,极高危;2型糖尿病。
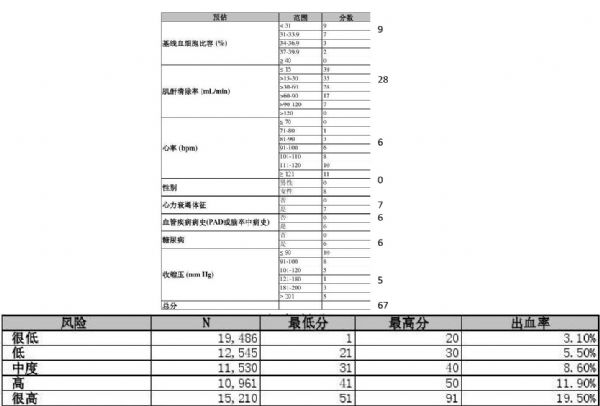
出血风险评估(Crusade评分):
缺血风险评估:
低危 ≤99,高危 100-200,极高危≥201
初步治疗方案
(1)早期侵入策略
(2)择期完全血运重建
药物治疗:
·阿司匹林 300mg-100mg qd
·替格瑞洛 180mg-90mg Bid
·阿托伐他汀钙片20 mg qd
·坎地沙坦酯片8 mg qd
·氨氯地平 5 mg qd
·呋塞米 20 mg qd
·螺内酯 20 mg qd
·生物合成人胰岛素皮下注射
出院带药:
·阿司匹林100 mg qd
·替格瑞洛90 mg Bid
·阿托伐他汀钙片20 mg qd
·坎地沙坦酯片8 mg qd
·氨氯地平 5 mg qd
·呋塞米 20 mg qd
·螺内酯 20 mg qd
·生物合成人胰岛素皮下注射
第二次入院
就诊时间: 2017年8月20日
患者主诉:主因心悸、乏力一周。
体格检查:神清语利,贫血貌,BP 110/95 mmHg,双肺呼吸音粗,未闻及明显干湿罗音,心界稍左侧扩大,心律齐,心率100次/分左右,心音低钝,双下肢无明显水肿。
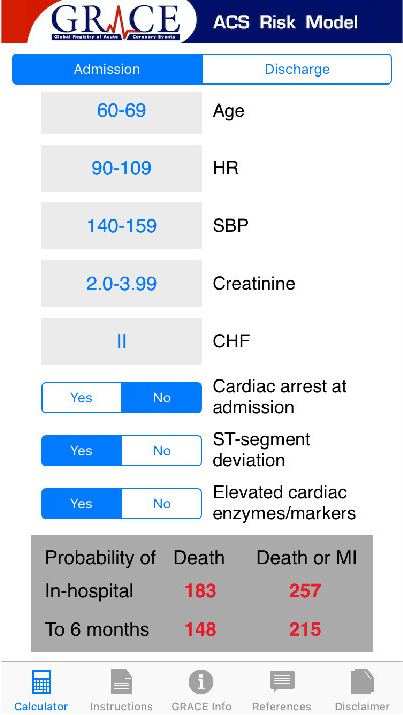
Crusade评分:
Grace评分:
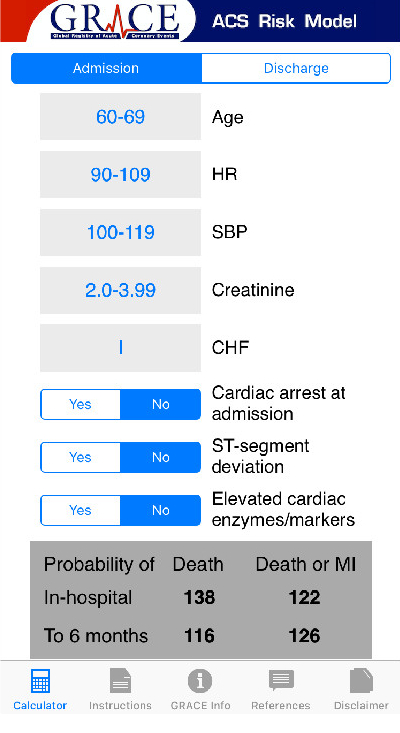
低危 ≤99,高危 100-200,极高危≥201
入院诊断:缺血性心肌病 (心力衰竭 心功能Ⅳ级);高血压病3级,极高危 ;2型糖尿病;十二指肠溃疡 (消化道出血 失血性贫血),急性支气管炎。
入院治疗方案:
(1)悬浮红细胞输入纠正贫血
(2)“四联抗HP治疗”
·停用 替格瑞洛 90 mg 2/日
·停用 阿司匹林 100 mg qd
·阿托伐他汀钙片 20 mg qd
·坎地沙坦酯片 8 mg qd
·氨氯地平 5 mg qd
·生物合成人胰岛素皮下注射
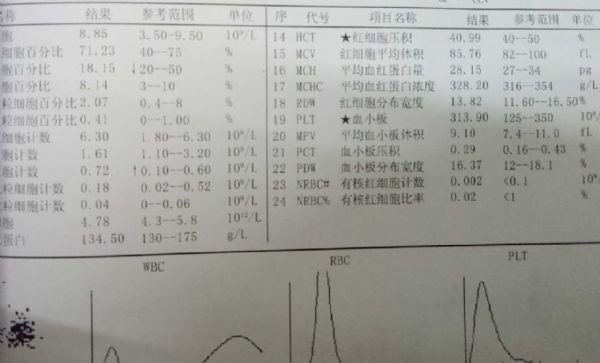
一周后复查血常规:
出院带药:
·氯吡格雷 75 mg qd
·阿托伐他汀钙片 20 mg qd
·坎地沙坦酯片 8 mg qd
·氨氯地平 5 mg qd
·呋塞米 20 mg bid
·螺内酯 20 mg qd
·雷贝拉唑钠肠溶片 20 mg qd
·生物合成人胰岛素 皮下注射
出院一周后门诊复查便潜血阴性,血红蛋白14g/L,加用阿司匹林 100 mg qd
第三次入院
就诊时间: 2018年2月7日。
患者主诉:主因心悸一周、突发左侧肢体无力、言语不清2小时。
体格检查:神清,言语含糊不清,T 36.7℃ P 150次/分 R 20次/分,BP 144/104 mmHg,双肺呼吸音清,心界左侧扩大,心律不齐,心音强弱不定,心室率160 次/分左右,心音低钝,双下肢无明显水肿。
入院诊断:经颅脑CT平扫与DWI检查诊断为急性脑栓塞;缺血性心肌病:心律失常、心房颤动、心力衰竭、心功能Ⅲ级;高血压病3级,极高危;2型糖尿病。
出血/缺血风险评估表
HAS-BLED评分: 8(高危)
CHA2DS2VASc 积分:6 (建议OAC)
入院治疗方案:
·氯吡格雷 75 mg qd
·达比加群酯 110 mg Bid
·阿托伐他汀钙片 20 mg qd
·坎地沙坦酯片8 mg qd
·氨氯地平 5 mg qd
·呋塞米 20 mg Bid
·螺内酯 20 mg qd
·生物合成人胰岛素,皮下注射
住院两周左侧肢体肌力恢复尚可,好转出院
PCI术后12个月复查后调整治疗方案:
·达比加群酯 110 mg Bid
·阿托伐他汀钙片 20 mg qd
·坎地沙坦酯片 8 mg qd
·氨氯地平 5 mg qd
·呋塞米 20 mg Bid
·螺内酯 20 mg qd
·生物合成人胰岛素 皮下注射
第四次入院
就诊时间: 2018年8月16日
患者主诉:乏力、心悸伴黑便3天入院。
体格检查:神清语利,BP 110/70 mmHg,双肺呼吸音稍低,双下肺可闻及湿罗音,心界左侧扩大,HR 90次/分左右,心律不齐,心音低钝,强弱不定,双下肢轻度指凹性水肿。
入院诊断:缺血性心肌病(心律失常 心房颤动,心力衰竭 心功能Ⅲ级);消化道出血;高血压病3级,极高危;2型糖尿病。
调整治疗方案:
·停用达比加群酯 110 mg Bid
·坎地沙坦酯片 8 mg qd
·氨氯地平 5 mg qd
·雷贝拉唑钠 80 mg iv qd
·生物合成人胰岛素 皮下注射
·压积红 2 u iv
·监测便潜血 血常规 生命体征
变更用药方案及随访:
·吲哚布芬片 50mg Bid
·坎地沙坦酯片 8mg qd
·氨氯地平 5 mg qd
·呋塞米 20mg bid
·螺内酯 20mg qd
·生物合成人胰岛素 皮下注射
·监测便潜血 血常规 生命体征
一周后出院:
·吲哚布芬片 100mg Bid
·坎地沙坦酯片 8mg qd
·氨氯地平 5 mg qd
·呋塞米 20mg bid
·螺内酯 20mg qd
·生物合成人胰岛素 皮下注射
本例患者单用达比加群治疗仍再发消化道出血,进一步抗栓选择选用吲哚布芬后病情稳定,随访未再发缺血/出血事件。
一周后病情稳定,复查血常规(如下图)
随访情况(出院四周)
临床启发
冠心病为常见多发病,抗血小板治疗为冠心病为常规治疗方案,目前主要用药为阿司匹林氯吡格雷,但因其胃肠道损伤不良反应,在一些特殊人群中应用受限, 临床治疗过程中应根据患者个体情况选择最佳抗栓策略及用药,并根据病情变化及时调整治疗方案,平衡缺血/出血风险,改善患者预后。
吲哚布芬可以通过多途径抑制血小板血小板聚集,并具有一定的抗凝作用,对动脉及静脉血栓形成均有有效抑制作用。同时无阿司匹林非甾体抗炎药胃肠道刺激作用,更少的不良反应,对于动脉硬化相关心脑血管、外周动脉疾病以及下肢静脉血栓形成具有很好适应症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#消化道#
26
好
84
很受用,谢谢!
71
学习了很有用不错
84
学习学习学习
81
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
33