本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

患者女,49岁。因“10d前出现构音障碍、四肢不自主颤动”收治入院。
48岁,男性。心肺复苏后出现管状视野。
骨质疏松性椎体压缩性骨折(OVCFs)是导致腰痛和行动能力丧失的一个常见问题。置入许多固定器具的传统开放式手术因疏松的骨质固定性不好而经常失败。 经皮椎体成形术(VP)是一种安全有效的治疗手段。经典的VP通过双侧经椎弓根或椎弓根外将骨水泥注入。许多学者将VP的技术挑战视为重度椎体压缩性骨折的相对或绝对禁忌症。然而,最近有研究报道称单侧VP可以达到同样的疗效。理论上来讲,单侧VP可以减少手
女,31岁。因“头痛、恶心17h,被人发现意识不清2h”于2015年10月8日入院。
人工全膝关节置换术(TKA)是是一种疗效确切、成本效益良好的常见外科手术。随着人口老龄化和手术指征的扩大,预计未来二十年TKA的手术需求将会有明显增长。这些患者往往同时双侧膝关节受累,因此医生和患者需要决定应该采用同期双侧TKA还是分次手术。 同期双侧TKA的潜在优势主要在于缩短了住院日、更短的麻醉时间、更短的康复时间及更少的医疗费用,除此以外,同期双侧TKA在功能结果、放射学结果、疼痛
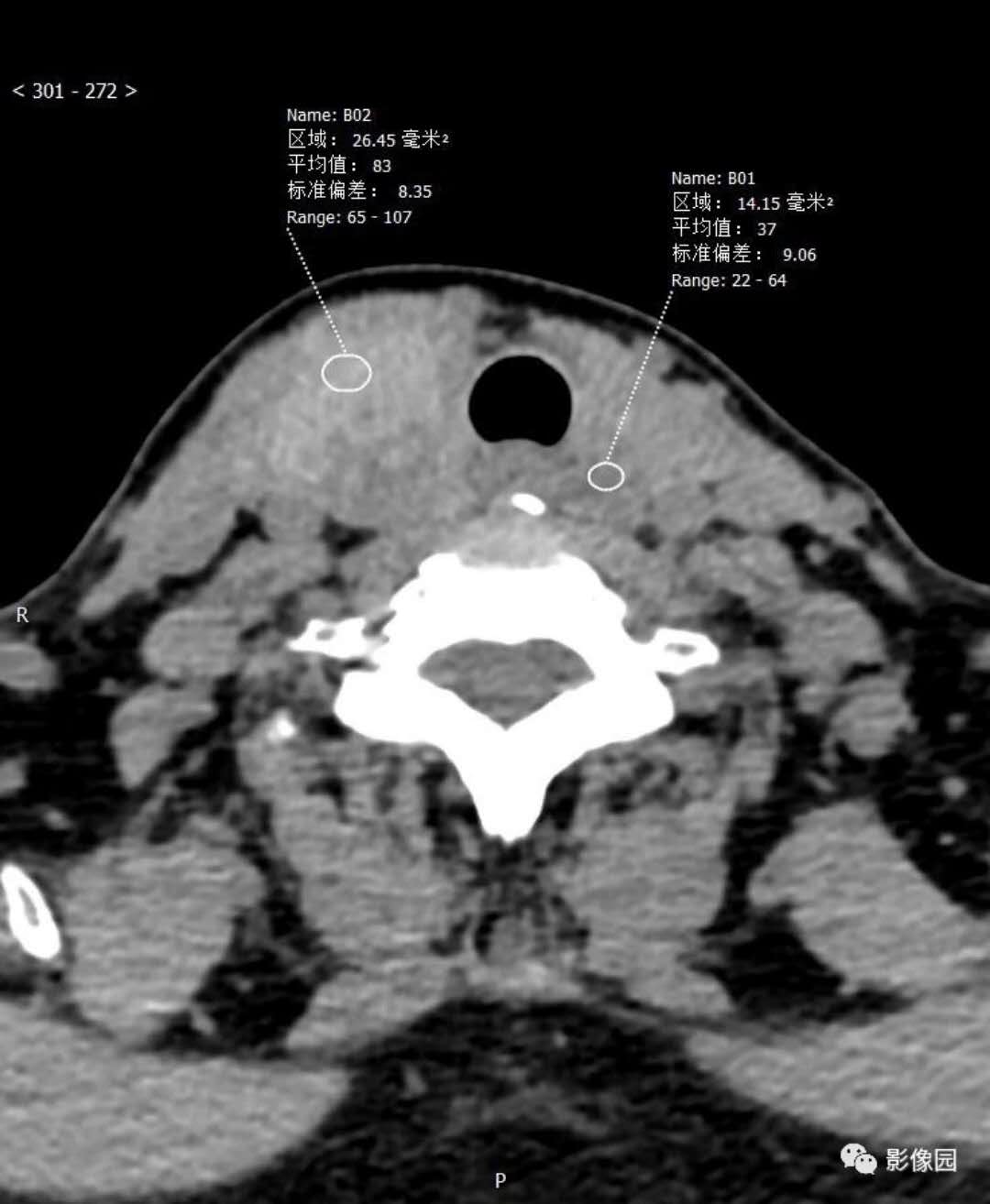
双侧输卵管异位妊娠是一种特殊的临床状态,其发病率约为自然妊娠的1/200000 。而体外受精异位妊娠的发病率约占所有临床妊娠的2.1%-9.4%。据报道,仅有一小部分双侧异位妊娠的患者在接受药物治疗后能正常宫内妊娠,并且成功分娩。 目前,有关卵细胞浆内单精子注射和胚胎移植(ICSI-ET)后双侧输卵管异位妊娠的病例报道很少,输卵管异位妊娠发病率的相关数据还不完善。Mehtap Polat


梅斯医学MedSci APP
医路相伴,成就大医
学习了
61
#双侧#
32
嗯嗯,学习了。
59
学习了
67