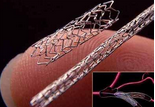
JACC:依维莫司洗脱支架的长期安全性优于西罗莫司洗脱支架
2016-02-16 崔倩 译 MedSci原创
依维莫司洗脱支架(EES)与那些西罗莫司洗脱支架(SES)相比的长期安全性和有效性是未知的。这项研究比较了SORT OUT IV试验(斯堪的纳维亚临床结果随机试验)中SES患者与EES患者5年的成果。五年随访期间研究人员完成了2771例(99.9%)患者的随访。主要终点为主要不良心脏事件(MACE),包括心源性死亡,心肌梗死(MI),靶血管血运重建(TVR),以及明确的支架内血栓形成的复合终点。在
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#洗脱支架#
30
#JACC#
28
#依维莫司洗脱支架#
33
#长期安全性#
36
#ACC#
25
#西罗莫司#
25