PRS:当前对乳房植入物的安全性和实用性的看法
2021-03-14 MedSci原创 MedSci原创
改进的方框标签可以提高非专业女性对乳房植入物安全性及效用的看法,并影响决策。然而,对乳房植入物的更严格的审查不应该阻止需要隆胸的女性接受隆胸。 鉴于乳房植入物在乳房重建和隆胸中发挥着重要作用,医生们应
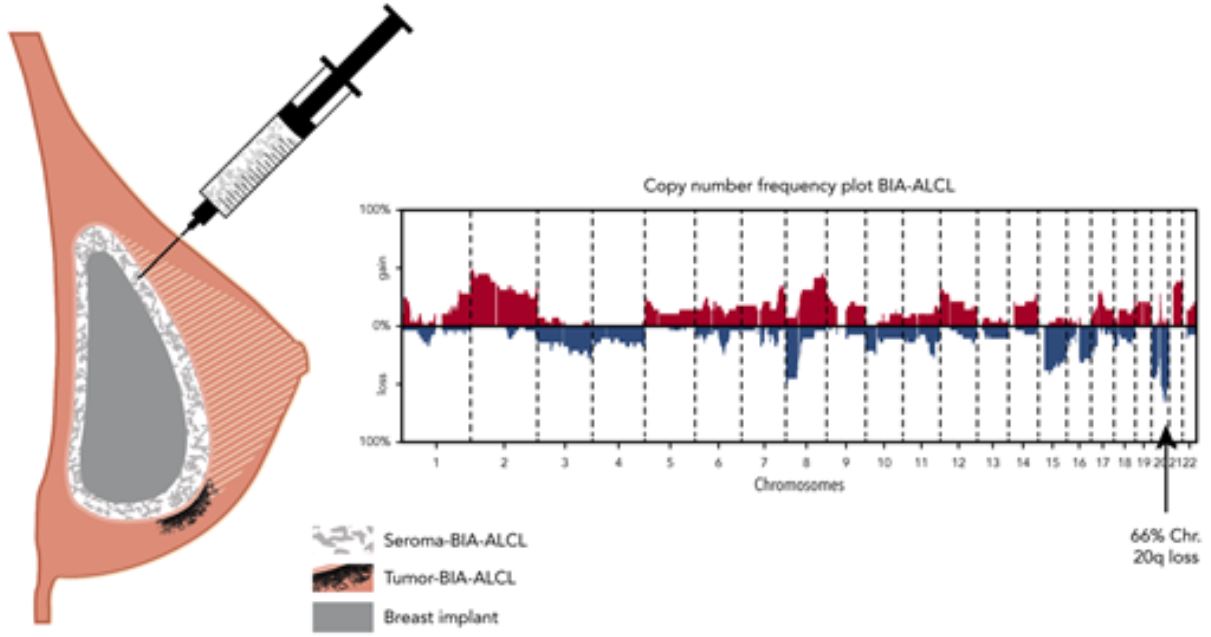
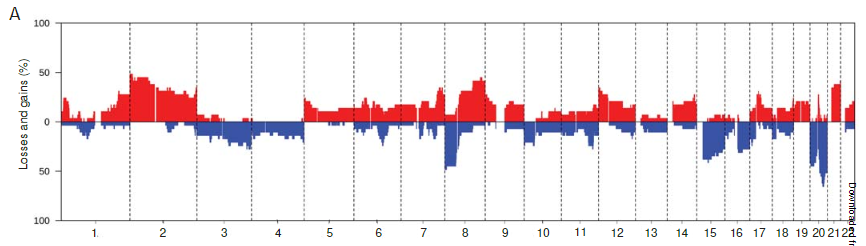
关于乳房植入物与间变性大细胞淋巴瘤(BIAALCL)相关的证据越来越多,使得乳房假体的安全性成为一个突出的问题。仅在美国就有300多例BIA-ALCL病例被记录在案,无数其他妇女报告了与乳房假体相关的全身症状,统称为乳房假体疾病。
尽管如此,假体乳房手术仍是整形外科医生最常进行的手术之一。因此,美国食品和药物管理局(FDA)已经采取措施。通过普通和整形外科设备咨询小组以及随后召回Allergan Biocell假体。在美国食品和药物管理局(FDA)介入后,公众对乳房植入物安全性的担忧与日俱增。事实上,美国食品和药物管理局(U.S.Food and Drug Administration,简称FDA)最近建议对隆胸标签进行修改,其中包括方框警告。

鉴于提高乳房植入物安全透明度的努力,该研究评估了非专业女性对乳房植入物安全性的看法,以及乳房植入物标签拟议的改变对非专业女性乳房植入物决策的影响。
这是一项针对通过Amazon Mechanical Turk. 论坛所招募女性的横断面调查。离散选择建模用于在查看建议的标签更改后,查询受试者对乳房植入物的意见。亚组分析使用卡方和方差分析,McNemar分析用于评估参与者反应的变化。
作者共收到500份调查问卷。在基线时,353名参与者(70.6%)认为隆胸至少在一定程度上是安全的。在基线时,353名参与者(70.6%)认为乳房植入物至少在一定程度上是安全的。此外,参与者对乳房植入物作为医疗设备的看法因其个人植入物历史而有显著差异(p<0.001)。
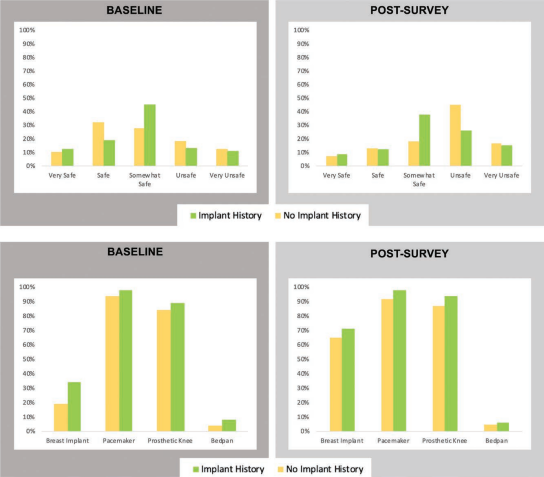
在看到拟议的方框警告后,252名参与者(50.4%)回应说,他们接受植入物的可能性较小。
事实上,在观看了对植入物标签的建议更改后,认为隆胸不安全或非常不安全的参与者比例明显高于基线(58.4%对28.8%;p=0.001)。在调查结束时,考虑隆胸/再造的替代方案的意愿比基线显著增加。
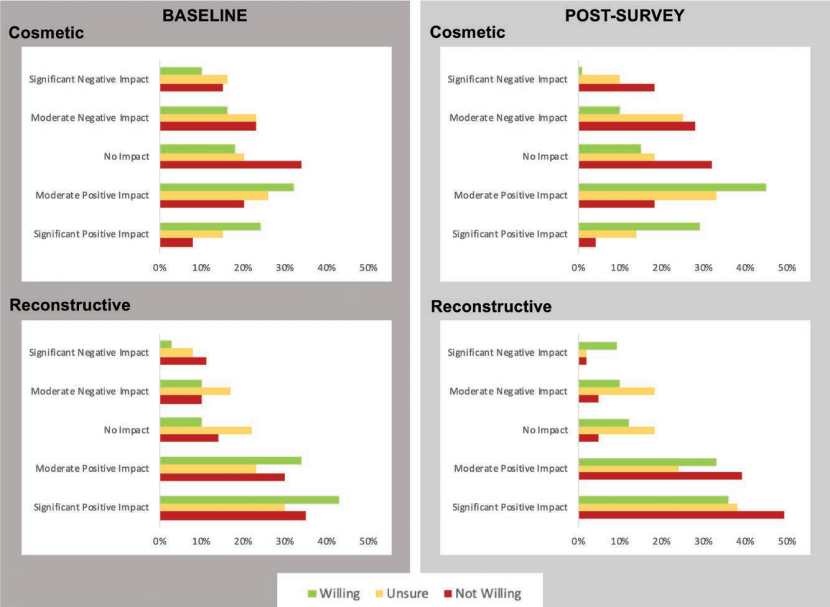

改进的方框标签可以提高非专业女性对乳房植入物安全性及效用的看法,并影响决策。然而,对隆胸的更严格的审查不应该阻止需要隆胸的女性接受隆胸。
鉴于乳房植入物在乳房重建和隆胸中发挥着重要作用,医生们应该确保未来的对话继续围绕乳房植入物最显著的风险和好处展开。外科医生和患者对话的透明度和客观性可以确保适当使用乳房植入物等医疗设备。
原始文献:
Yesantharao Pooja S,Lee Erica,Khavanin Nima et al. Thinking Outside the Black Box: Current Perceptions on Breast Implant Safety and Utility.[J] .Plast Reconstr Surg, 2021, 147: 593-603.
DOI: 10.1097/PRS.0000000000007626
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PRS#
36
#乳房植入#
54
#实用性#
48
适度医疗
88
#植入物#
56
#植入#
34