JAMA OHNS:鼻窦球囊扩张在药物治疗抵抗的儿童慢性鼻窦炎治疗中的应用
2015-04-07 Zhang JL译 MedSci原创
儿童慢性鼻窦炎(CRS)在临床很常见,其对孩子的生活质量和学习能力产生不少负面影响。该病可能由多种因素导致,包括细菌感染以及炎症因素。在儿童群体中,腺样体肥大是儿童CRS的一个重要诱因。目前,CRS的主要治疗方法为抗生素治疗加上局部或系统性皮质类固醇治疗和盐水灌洗。一半以上的患儿在接受腺样体切除术后CRS的症状或预后有所改善。然而,有些患儿尽管接受手术治疗以及最大限度的药物治疗,但其CRS症状持续
儿童慢性鼻窦炎(CRS)在临床很常见,其对孩子的生活质量和学习能力产生不少负面影响。该病可能由多种因素导致,包括细菌感染以及炎症因素。在儿童群体中,腺样体肥大是儿童CRS的一个重要诱因。目前,CRS的主要治疗方法为抗生素治疗加上局部或系统性皮质类固醇治疗和盐水灌洗。一半以上的患儿在接受腺样体切除术后CRS的症状或预后有所改善。然而,有些患儿尽管接受手术治疗以及最大限度的药物治疗,但其CRS症状持续并有进一步接受手术干预的需要。
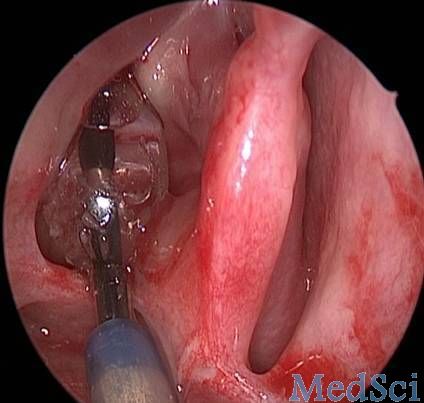
鼻窦球囊导管扩张(SBCD)对于上颌窦、额窦、蝶窦CRS的治疗自2006年引进以来,已在多中心的成年人研究中被证明是安全有效的。它也被用于治疗儿童CRS并且使手术的有效性从单纯腺样体切除术的50%增加增加至80%。然而,目前鲜有关于SBCD应用于治疗儿童CRS较为全面的病例对照研究报道。
为研究SBCD对于儿童CRS治疗的有效性,研究人员对一个三级教学医院的患儿进行前瞻性病例对照研究。该研究入组96例患儿,就诊时间为2012年10月1日至2013年5月31日,年龄在7到12岁,均为CRS药物治疗抵抗。
研究人员对入组患儿的年龄、性别、计算机断层扫描的结果、SBCD治疗(病例组)或保守治疗(对照组)、sinonasal-5问卷(SN-5)和视觉模拟量表(VAS)等方面进行了分析和比较。
在96名入组的患儿中,有79名患儿完成随访文件并进行统计分析(其中包括42名男孩,37名女孩平均年龄(SD)为9.3(1.7)岁)。与术前相比分数,接受SBCD有或无进行腺样体切除术的CRS儿童的SN-5和VAS评分在治疗后3个月显著降低 (SN-5:2.5 vs 4.3,P<0.001;VAS:3.1 vs 5.2,P<0.001),治疗后1年也是显著降低(SN-5:2.9vs 4.3,P=0.001;VAS:3.1 vs5.2,P<0.001)。对照组的SN-5和VAS评分在治疗3个月后显著降低(SN-5:3.1vs 4.2,P= 0.001;VAS:3.9vs 5.1,P<0.001),但在治疗后12个月变化不明显(SN-5:3.8vs 4.2,P=0.01;VAS:4.9vs 5.1,P= 0.54)。SBCD组的SN-5和VAS评分显著低于对照组在3个月(SN-5:2.5vs 3.1;P=0.003;VAS:3.1vs 3.9,P=0.01)和在手术后1年(SN-5:2.9vs 3.8,P<0.001;VAS:3.1 vs4.9,P<0.001)。通过术后12个月的SN-5分数评估,SBCD组的显著、中等和轻度改善 (52%[42中的22],26%[42中的11],和14%[42中的6]均比对照组(14%[37中的5],19%[37中的7],和11%[37中的4])(所有的比较差异P < 0.05)显著。
因此,SBCD对于药物治疗抵抗的儿童CRS是一种安全、有效的治疗技术。
原始出处:
Wang F, Song Y, Zhang X, Tan G. Sinus Balloon Catheter Dilation in Pediatric Chronic Rhinosinusitis Resistant to Medical Therapy. JAMA Otolaryngol Head Neck Surg. Published online April 02, 2015. doi:10.1001/jamaoto.2015.0397.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#球囊扩张#
31
#扩张#
35
#慢性鼻窦炎#
41
#球囊#
29