Nature、Cell两篇文章发现10种用于疾病诊断的CRISPR酶
2017-05-06 生物谷 生物谷
最近来自加利福尼亚大学的研究人员通过研究描述了10种新型的CRISPR酶,这些酶一旦被激活其行为就像“吃豆人”一样能够“嚼碎”RNA,因此这些酶类或许能作为诊断传染性病毒的敏感检测器。这种新型的酶类是CRISPR蛋白—Cas13a的突变体,
电脑绘制出的RNA分子。图片摘自:Richard Feldmann/Wikipedia
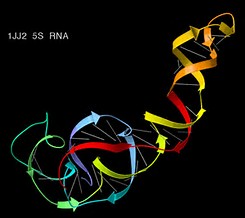
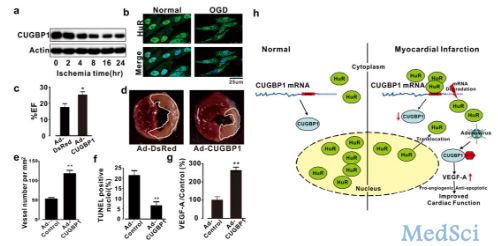
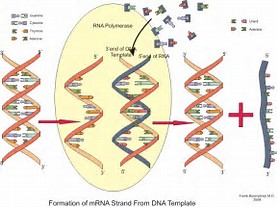
最近来自加利福尼亚大学的研究人员通过研究描述了10种新型的CRISPR酶,这些酶一旦被激活其行为就像“吃豆人”一样能够“嚼碎”RNA,因此这些酶类或许能作为诊断传染性病毒的敏感检测器。这种新型的酶类是CRISPR蛋白—Cas13a的突变体,去年9月,来自伯克利的研究人员利用该蛋白实现了对来自病毒RNA的特异性序列进行检测,同时研究者表示,一旦CRISPR—Cas13a同其靶点RNA相结合后,其就会开始切割RNA,从而就能够轻松切掉和受体分子相关的RNA,并且产生荧光帮助研究者进行信号检测。
此前来自博德研究所的两个研究小组相继对CRISPR—Cas13a和RNA进行配对,并将构建好的新系统命名为SHERLOCK系统,该系统能够在极低浓度下对病毒的RNA进行检测,比如对登革热和寨卡病毒的RNA进行检测等。诸如这种系统就能够用来检测任何类型的RNA,包括癌细胞特异性的RNA
当伯克利和博德研究所的研究人员发现使用的原始的Cas13a酶仅能够在特定核苷酸位点(尿嘧啶)对RNA进行切割时,本文中研究者发现了其中三种新型的Cas13a突变体则能够在腺嘌呤位点切割RNA,这种差异性就能够实现同时检测两种不同的RNA分子,比如来自两种不同病毒的RNA。研究者Alexandra East-Seletsky表示,我们通过深入研究发现了具有不同核苷酸的Cas13a家族的其它同系物,这就能够对携带红色和绿色荧光信号的不同受体分子进行同时检测,从而帮助研究者开发多通道的酶类检测系统。
研究者East-Seletsky表示,把Cas13a与RNA靶点结合看作一种开关,靶向作用该开关就能够开启酶类的表达使其成为细胞中的“吃豆人”来切割附近的RNA分子。发表在Nature杂志上的研究报告中,伯克利的研究人员讨论了CRISPR—Cas13a所具有的活性是否能在细菌中扮演关键角色,从而帮助细菌杀灭感染性的病毒或噬菌体,作为一些细菌的部分免疫系统组分,CRISPR—Cas13a能够促进感染的细胞自杀从而帮助抵御其它细菌细胞免于被感染,类似的非CRISPR自杀细菌在其它其中中也存在。
随后研究人员对细菌基因组数据库进行搜寻,发现了10个其它的Cas13a样蛋白,随后研究者对这些蛋白进行了合成,并且评估其切割RNA的能力,其中有7个蛋白类似原始的Cas13a,另外3个则能够对RNA进行切割。基于前期的研究结果,研究人员表示,他们或许能够多元化地使用这些酶类,并且扩展该技术的使用范围,CRISPR-Cas13a家族或许还有其它多种用途,比如进行RNA检测等。最后研究者Doudna说道,我们未来的研究目的就是开发用于多个医疗点诊断的强大Cas13a酶类家族。
原始出处:
Alexandra East-Seletsky,Mitchell R. O’Connell,Spencer C. Knight, et al. Two distinct RNase activities of CRISPR-C2c2 enable guide-RNA processing and RNA detection. Nature 538, 270–273 (13 October 2016) doi:10.1038/nature19802.
Alexandra East-Seletsky, Mitchell R. O’Connell, David Burstein, et al. RNA Targeting by Functionally Orthogonal Type VI-A CRISPR-Cas Enzymes. Molecular Cell (2017) doi:10.1016/j.molcel.2017.04.008
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
27
#Nat#
35
#疾病诊断#
39
#CEL#
33
#CRISPR#
32