Obstet Gynecol:AFP与胎膜早破
2015-01-16 Mechront 译 MedSci原创
众所周知,胎膜早破与宫内感染和早产儿发生率密切相关,在美国,每年约有3%的孕妇经历胎膜早破,对其进行早期诊断和干预是降低并发症的关键所在。目前临床上常用的诊断方式存在低特异性和低阳性预测值,因此Amir Mor等人进行了一项前瞻性队列研究,以探究能否使用羊水中甲胎蛋白(AFP)含量作为胎膜早破的标志。 该研究纳入52例尿液样本、52例羊水样本,均来自52名顺产孕妇。17例精液样本,来自17名
众所周知,胎膜早破与宫内感染和早产儿发生率密切相关,在美国,每年约有3%的孕妇经历胎膜早破,对其进行早期诊断和干预是降低并发症的关键所在。目前临床上常用的诊断方式存在低特异性和低阳性预测值,因此Amir Mor等人进行了一项前瞻性队列研究,以探究能否使用羊水中甲胎蛋白(AFP)含量作为胎膜早破的标志。
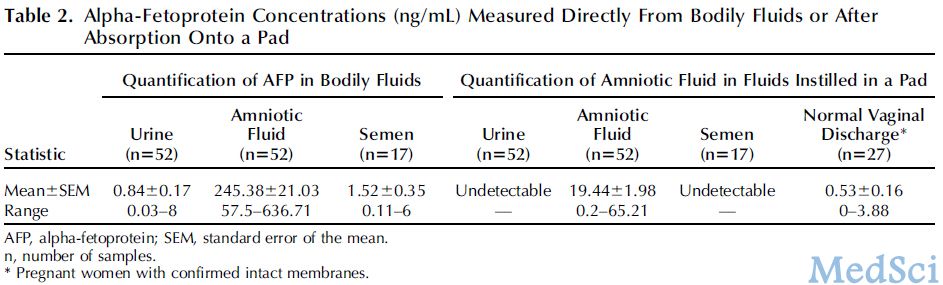
该研究纳入52例尿液样本、52例羊水样本,均来自52名顺产孕妇。17例精液样本,来自17名进行不孕不育评估的男性。27例正常阴道分泌物样本,来自27名孕妇的卫生巾。研究分别检测了尿液、羊水、精液中AFP浓度,以及从卫生巾提取的尿液、羊水、精液和阴道分泌物中AFP浓度。最新研究成果发表在2015-01-07 Obstet Gynecol 杂志社,证据等级为II级。
研究结果表明,羊水中AFP浓度(245.38±21.03 ng/mL, n=52)明显高于尿液(0.84±0.17 ng/mL,n=52, P,.001)、精液(1.52±0.35 ng/mL, n=17,P,.001)。同样从卫生巾上提取物检测AFP浓度也得到类似结果:羊水中AFP浓度(19.44±1.98ng/mL, n=52)明显高于尿液(undetectable, n=52)、精液(undetectable,n=17)、正常阴道分泌物(0.53±0.16 ng/mL,n=27, P,.001)。受试者工作特征曲线分析显示通过该方法区分卫生巾上阴道分泌物和羊水的灵敏度为96.2%,特异度为100%(阈值3.88 ng/mL,曲线下面积 0.99)。
该研究认为,当可疑胎膜早破诊断时,测定AFP浓度可以判断该物质是否为羊水。该研究提供了准确方便的胎膜早破诊断方法:只需要对卫生巾上的物质定量测定AFP浓度,即可对可以胎膜早破进行诊断。
本文是MedSci原创编译整理,欢迎转载!转载请注明来源并附原文链接。谢谢!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#NEC#
34
#AFP#
33
#TET#
33
#胎膜早破#
40