JAMA Netw Open:开发和验证治疗效益指数,以确定COVID-19住院患者谁可能受益于恢复期血浆
2022-01-31 从医路漫漫 MedSci原创
确定哪些COVID-19患者可能受益于COVID-19恢复期血浆(CCP)治疗,可能会对公共卫生产生重大影响。
确定哪些COVID-19患者可能受益于COVID-19恢复期血浆(CCP)治疗,可能会对公共卫生产生重大影响。建立一种指标,利用患者基线特征预测COVID-19住院患者使用CCP与不使用CCP治疗的预期相对疗效。
本预后研究使用了COMPILE研究的数据,即荟萃分析了8个随机临床试验(rct)的个体患者数据,评估了COVID-19住院且未接受机械通气的成人患者的CCP与对照。一种基线特征的组合被称为治疗受益指数(TBI),该组合基于COMPILE中的2287例患者,使用比例优势模型,通过交叉验证选择基线特征。TBI通过4个外部数据集进行外部验证:扩展访问计划(1896名参与者)、一项在紧急使用授权下进行的研究(210名参与者)和2项随机对照试验(80名参与者和309名参与者)。接收CCP。
随机分组后第14天和第28天,世界卫生组织(WHO) 11点序贯COVID-19临床状态量表及其2个衍生量表(WHO评分7-10,表示机械通气死亡;WHO评分10,表示死亡)。第14天采用WHO 11点顺序量表作为TBI发展的主要结局。
共2287例患者纳入衍生队列,平均年龄(SD) 60.3岁(15.2岁),女性815岁(35.6%)。TBI提供了一个持续的获益分级,并且,为了临床效用,它被操作化为预期的大临床获益组(B1;派生队列中629名参与者[27.5%],中度获益(B2;953[41.7%]),以及潜在的危害或无益处(B3;705[30.8%])。预计有既往病史(糖尿病、心血管和肺部疾病)、血型为A型或AB型并处于COVID-19早期阶段(世卫组织基线评分较低)的患者受益最大,而那些没有既往病史和处于COVID-19较晚期阶段的患者则可能受到损害。在衍生队列中,较差结局的优势比为:B1为0.69(95%可信区间[CrI] 0.48-1.06),B2为0.82(95%可信区间[CrI] 0.61-1.11), B3为1.58 (95% CrI, 1.14-2.17)。在4个外部数据集上的测试支持派生TBI的验证。

图1 COVID-19恢复期血浆(CCP)疗效与扩大治疗效益指数的比值比

图2.3个受益组的死亡时间和28天内出院时间
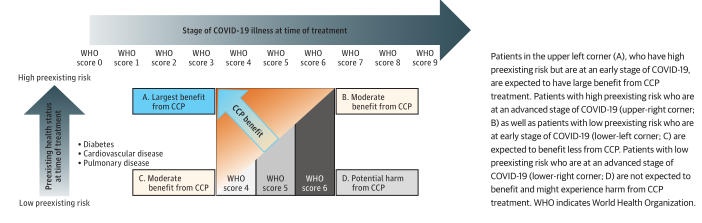
图3.先前存在的健康状况、治疗时新冠肺炎疾病的阶段以及从新冠肺炎恢复期血浆(CCP)中获益
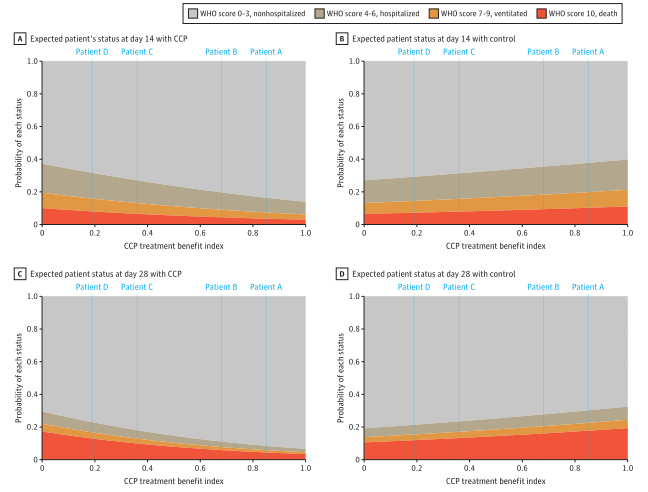
图4.4个样本患者的预测患者状态
本研究的结果表明,CCP TBI是一种简单的工具,可以量化CCP治疗对COVID-19住院患者个体的相对益处,可用于指导治疗建议。TBI精准医疗方法在大流行中尤其有用。
原文出处:Park H, Tarpey T, Liu M,et al.Development and Validation of a Treatment Benefit Index to Identify Hospitalized Patients With COVID-19 Who May Benefit From Convalescent Plasma.JAMA Netw Open 2022 Jan 04;5(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#NET#
50
#PE#
33
#恢复期#
47
#恢复期血浆#
43
学习
52