Cardiovasc Diabetol:CT血管成像时冠脉周围脂肪组织密度高可预测2型糖尿病患者的心血管事件
2022-04-28 从医路漫漫 MedSci原创
在冠状动脉CTA上评估的冠状动脉周围脂肪组织(PCAT)衰减的变化被引入作为炎症的新指标。
背景:冠状动脉疾病(CAD)是二型糖尿病糖尿病(T2DM)患者死亡的主要原因。随着T2DM在全球的日益流行,作为一项公共卫生措施,预防T2DM患者的冠心病变得越来越重要。冠状动脉计算机断层造影(CTA)是评估T2DM患者冠心病的一种有用的诊断方法。冠状动脉CTA评估中显示阳性重塑和低斑块密度的动脉粥样硬化斑块与未来心血管事件的高风险相关;然而,总的来说,这些经CTA验证的斑块特征预测心血管事件的预后价值有限。因此,需要一种诊断方法来帮助识别易发生心血管事件的T2DM患者。
最近,在冠状动脉CTA上评估的冠状动脉周围脂肪组织(PCAT)衰减的变化被引入作为炎症的新指标。在使用计算机断层造影(CRISP-CT)进行的心血管风险预测研究中,左前降支动脉(LAD)和右冠状动脉(RCA)周围的高PCAT衰减被证明是增加心脏死亡率的一个重要风险因素。此外,PCAT衰减评估导致心血管风险和预测风险的显著改善,优于单独冠状动脉CTA的特征。因此,PCAT衰减已被确定为心血管风险的新标志。尽管PCAT衰减有可能增强临床风险评估,但迄今为止很少有研究调查PCAT衰减的预后价值。因此,需要进一步的研究,包括更大的研究人群,包括T2DM患者,以证实PCAT衰减的临床意义。
目的:本研究旨在探讨PCAT降低对2型糖尿病(T2 DM)患者预后的预测价值。
方法:对333例T2 DM患者(平均年龄66岁,男性211例,平均体重指数25 kg/m2)行冠状动脉CTA检查,检查冠状动脉钙化积分、心包脂肪体积、狭窄程度(管腔狭窄>50%)、斑块低密度和/或阳性重塑和/或点状钙化的高危斑块特征,以及PCAT衰减情况。我们评估了左前降支(LAD)和右冠状动脉(RCA)近端40 mm节段的Hounsfield单位(HU)的PCAT衰减。心血管事件被定义为心源性死亡、因急性冠脉综合征住院、晚期冠脉血管重建术和因心力衰竭住院。
结果:在中位数为4.0年的随访中,我们观察到31个心血管事件。有心血管事件组LAD-PCAT衰减显著高于无心血管事件组(−68.5±6.5HU vs−70.8±6.1HU,p=0.045),而RCAPCAT衰减无显著差异(p=0.089)。在包括不良−结果的模型中,LAD-PCAT的高衰减(>CTA 70.7HU;中位值)与心血管事件显著相关,例如显著狭窄和/或高风险斑块(危险比;2.69,95%可信区间;1.17-0.20,p=0.020)。在将LAD-PCAT衰减添加到不利的CTA发现后,C统计值和全局卡方值分别从0.65显著增加到0.7(p=0.037)和10.9-15.0(p=0.043)。
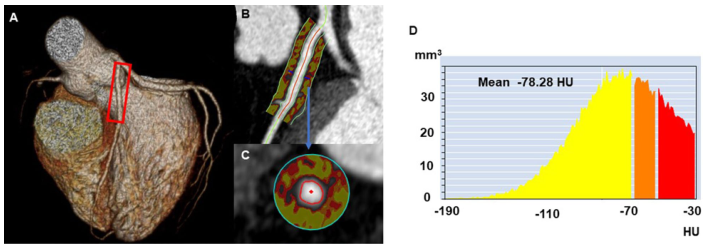
图1冠状动脉CT血管造影测量的冠状动脉周围脂肪组织衰减的典型病例。心脏的三维重建(A);在纵向视图(B)和横截面视图(C)中,冠状动脉周围脂肪组织衰减在190和–30 HU之间;左前降支近端40 mm左右;追踪区域内的CT衰减直方图(D)
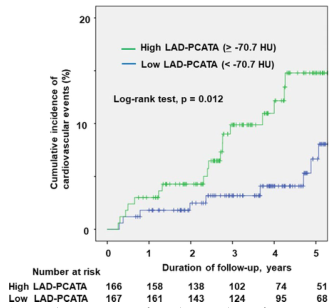
图2心血管事件累积发生率的卡普兰-迈耶曲线。Kaplan-Meier曲线与二型糖尿病病患者左前降支-冠状动脉周围脂肪组织衰减的高低有关。冠状动脉周围脂肪组织衰减
表1与心血管事件相关的因素
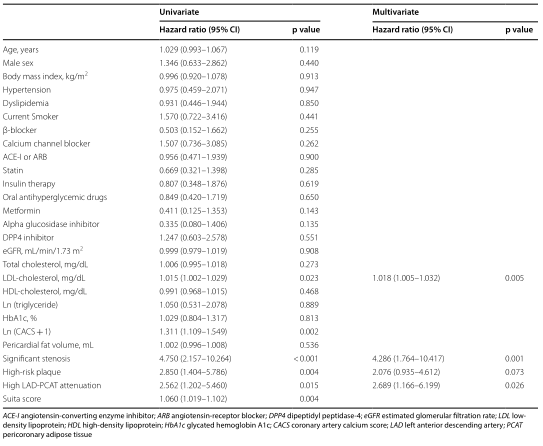
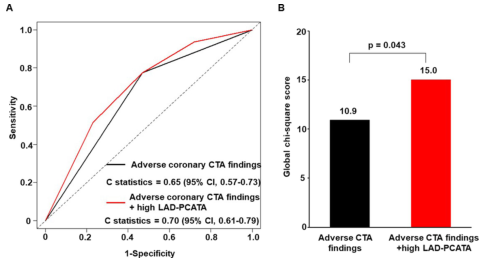
图3左前降支-冠状动脉周围脂肪组织衰减与不良冠状动脉CTA结果相比对预测心血管事件的增量预后价值。A.接收机工作特性曲线。B全球卡方检验。不利CTA发现、显著狭窄和/或高风险斑块;计算机断层血管造影术;冠状动脉周围脂肪组织衰减
结论:在接受临床诊断的冠状动脉CTA的T2 DM患者中,LAD-PCAT的高密度可以显著预测心血管事件。这表明评估LAD-PCAT衰减可以帮助医生识别高危T2 DM患者。
原文出处:Ichikawa K, Miyoshi T, Osawa K,et al.High pericoronary adipose tissue attenuation on computed tomography angiography predicts cardiovascular events in patients with type 2 diabetes mellitus: post-hoc analysis from a prospective cohort study.Cardiovasc Diabetol 2022 Mar 18;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#组织密度#
33
#DIA#
35
#血管成像#
51
#ASC#
45
#BET#
33
#血管事件#
36
#脂肪组织#
42
#2型糖尿病患者#
35
#糖尿病患者#
30
#学习#学习
71