BLOOD :通过与蛋白质翻译抑制剂和bcl2共同治疗具有RUNX1突变的AML的有效治疗
2021-10-05 MedSci原创 MedSci原创
BRM是一种细胞内在因子,它限制了HPCs的胞内缬氨酸,从而调节HPCs的增殖、存活、功能和线粒体代谢
RUNX1是一种参与正常和恶性造血功能的主调控转录因子。AML 中的大多数 RUNX1 突变是错义或缺失截断,表现为功能丧失突变。值得注意的是,突变体(mt)RUNX1可能会促进MDS和骨髓增生性肿瘤(MPN)中的白血病转化。在标准治疗后,表达 mtRUNX1 的 AML 患者比没有突变 RUNX1 的患者表现出较差的临床结果。
有提出的研究表明,与缺乏 mtRUNX1 的 AML 细胞相比,它们携带 mtRUNX1 的同基因对应物显示出核糖体生物发生和分化受损,以及野生型 RUNX1、PU.1 和 c-Myc 的水平降低。与只有野生型 RUNX1 的 AML 细胞相比,表达 mtRUNX1 的 AML 细胞对蛋白质翻译抑制剂高三尖杉酯碱(奥西他星)和 BCL2 抑制剂 venetoclax 也更敏感。
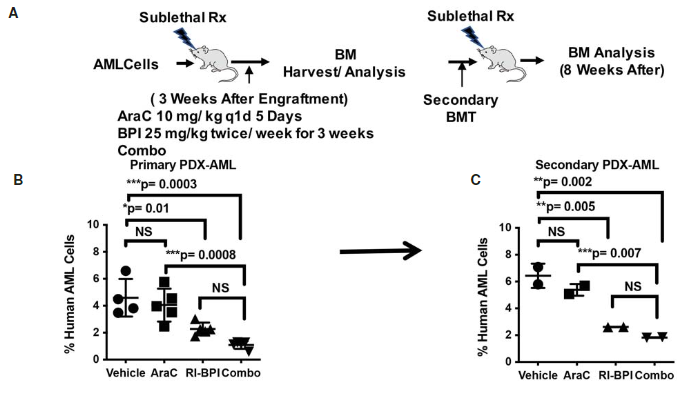
HHT 治疗抑制了增强子及其 BRD4 占据,并与 c-Myc、c-Myb、MCL1 和 Bcl-xL 水平降低有关。与此一致,奥美他星和维奈托克或 BET 抑制剂的共同治疗在表达 mtRUNX1 的 AML 中诱导协同体外致死率。与单独使用每种药物相比,奥美他星和 venetoclax 或 BET 抑制剂的联合治疗也显示出提高的体内抗 AML 功效,这与移植了带有 mtRUNX1 的 AML 细胞的免疫耗竭小鼠的存活率提高有关。
目前,AML预后亚型的ELN分类将具有mtRUNX1的AML指定为与不良预后相关的临时实体。这些发现强调了基于奥美他星的联合疗法对携带 mtRUNX1 的 AML 的优越疗效。因此,得到在这里讨论的临床前研究结果的支持,如果努力设计,未来基于om的静脉托和/或BET抑制剂联合临床试验进行并改善临床结果,那么可能有必要重新考虑mtRUNX1作为与不良前列腺相关的实体的AML单独命名。
原始出处:
Christopher P Mill, Warren Fiskus, Courtney D DiNardo, Christine Birdwell, John A Davis, Tapan Mahendra Kadia, Koichi Takahashi, Nicholas J Short, Naval G. Daver, Maro Ohanian, Gautam Borthakur, Steven M Kornblau, Michael R Green, Yuan Qi, Xiaoping Su, Joseph D. Khoury, Kapil N Bhalla; Effective therapy of AML with RUNX1 mutation by co-treatment with inhibitors of protein translation and BCL2. Blood 2021; blood.2021013156. doi: https://doi.org/10.1182/blood.2021013156
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#白质#
44
#抑制剂#
44
#蛋白质#
41
#BCL2#
37
#RUNX1#
45
#有效治疗#
42