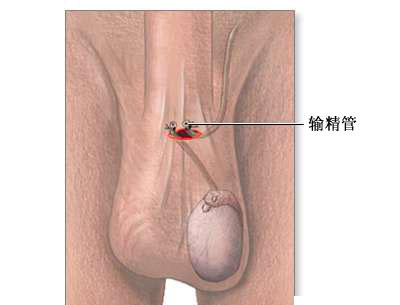
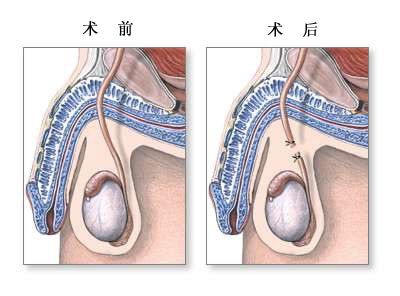
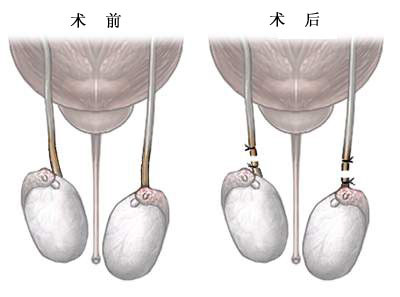
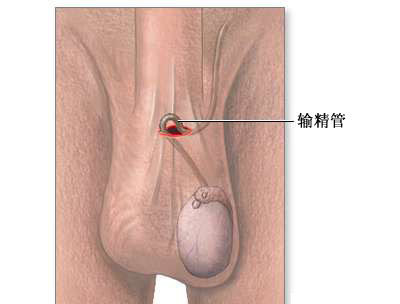
输精管结扎术是一个在门诊就可进行的小手术,并且短期并发症很少。这个小手术对于大多数男性而言是一个有效而且最可靠的长期避孕方法。全球估计有3300万妇女依靠其伴侣的输精管结扎术避孕,然而,一些研究表明输精管结扎术和前列腺癌之间可能存在相关性。最近,顶级杂志BMJ上发表了一篇来自加拿大多伦多大学玛格丽特公主癌症中心泌尿外科的Madhur Nayan医生及其团队的研究文章,旨在明确输精管结扎术和前列腺癌之间是否存在相关性。
该研究采用以人群为基础的匹配队列研究,检索了加拿大安大略省多个认证的医疗数据库在1994年至2012年期间的数据。该研究纳入了326,607名 年龄在20至65岁之间并接受了输精管结扎术的男性参与者作为试验组,同时,根据疾病评分、地域、1:1匹配没有接受输精管结扎术的男性作为对照组。
该研究的主要结局事件为前列腺癌发病率。次要结局事件为前列腺癌相关的分级、分期和死亡率。研究者发现在中位随访10.9年后共有3462例前列腺癌患者,其中输精管结扎术组患者有1843(53.2%)例前列腺癌患者,对照组有1619(46.8%)例。未经调整的分析结果显示,输精管结扎术导致前列腺癌的风险轻微增加(风险比为1.13,95%置信区间为1.05-1.20)。对影响因素进行调整后再分析显示,这种微弱的相关性也不复存在(调整后的风险比为1.02,95%置信区间为0.95-1.09)。此外,未发现输精管结扎术和恶性程度较高的前列腺癌(调整后的比值比为1.05,95%可信区间为0.67-1.66)、晚期前列腺癌(调整后的比值比为1.04,95%可信区间为0.81-1.34)或死亡(调整后的危险比为1.06,95%可信区间为0.60-1.85)之间存在相关性。
由此可见,本研究的结果并不支持输精管结扎术和前列腺癌之间存在独立的相关性。
原始出处:
Madhur Nayan, et al. Vasectomy and risk of prostate cancer: population based matched cohort study. BMJ 2016; http://dx.doi.org/10.1136/bmj.i5546
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#输精管结扎术#
28
#输精管#
41
有种怪怪的感觉
57
#BMJ#
21
#癌风险#
27
#前列腺癌风险#
23
有意思的研究
53