Cell:胶质瘤干细胞可能支持血管功能和肿瘤生长
2013-05-06 MedSci MedSci原创
来自美国克利夫兰医学中心、凯斯西储大学和厦门大学的研究人员在新研究中证实,胶质母细胞瘤干细胞生成血管周细胞,支持了血管功能和肿瘤生长。这一研究发现对于我们深入了解胶质母细胞瘤发病机制,开发出这一致命性疾病的靶向性新治疗策略具有重要的意义。相关论文发表在3月28日的《细胞》(Cell)杂志上。 领导这一研究的是克利夫兰医学
来自美国克利夫兰医学中心、凯斯西储大学和厦门大学的研究人员在新研究中证实,胶质母细胞瘤干细胞生成血管周细胞,支持了血管功能和肿瘤生长。这一研究发现对于我们深入了解胶质母细胞瘤发病机制,开发出这一致命性疾病的靶向性新治疗策略具有重要的意义。相关论文发表在3月28日的《细胞》(Cell)杂志上。
领导这一研究的是克利夫兰医学中心的华人科学家鲍仕登(Shideng Bao)博士,其现任厦门大学生命科学学院教授。主要研究方向包括细胞DNA损伤检控系统的信息传导,细胞周期检控系统功能失调与肿瘤发生的关系,肿瘤血管形成分子机理及其与肿瘤的发展,肿瘤的生物治疗和预防,干细胞技术及其在医学上的应用。
胶质母细胞瘤(Glioblastoma Multiform;GBM),世界卫生组织命名为4型神经胶质瘤。这种肿瘤生长快,病程短,是一种最常见的脑胶质瘤之一,占胶质瘤的25%以上,也是最恶性的一种。目前主要的治疗的方法就是手术切除与术后放疗等结合,由于至今未找到发病的关键环节,所以这些治疗方案都不尽如意,胶母细胞瘤的治愈率很低,存活期很短。
近年来,肿瘤干细胞学说的提出为肿瘤的产生和治疗提供了新的思路。已有许多证据表明,多种类型的胶质瘤组织中存在一群具有干细胞特性的细胞,称为胶质瘤干细胞(glioma stem cell,GSCs)。它与胶质瘤的发生发展密切相关。深入了解这些胶质瘤干细胞,对我们正确认识和理解脑胶质瘤的发生、发展及其生物学行为如侵袭性、转移、肿瘤的耐药性等均具有十分重要的理论意义和潜在的应用价值。
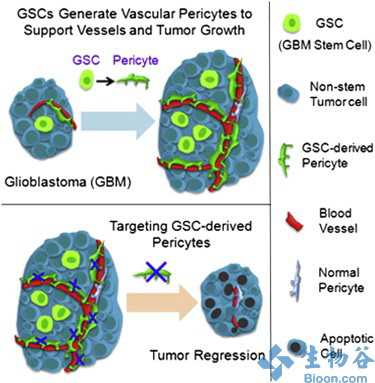
由于胶质瘤干细胞通常位于血管周围微环境(nich)中,有可能经历了间质分化,研究人员怀疑GSC是否有可能生成了血管周细胞。在这篇文章中,研究人员证实胶质瘤干细胞生成了周细胞,支持了血管功能和肿瘤生长。

在体内实验中,研究人员利用组成性和谱系特异性荧光报告系统进行细胞谱系追踪,证实胶质瘤干细胞生成了大多数的血管周细胞。当研究人员选择性除去胶质瘤干细胞源性周细胞时,发现其导致了新血管系统破坏,有力抑制肿瘤生长。分析人类胶质母细胞瘤样本,结果表明大部分周细胞都来源于瘤细胞。在进一步的机制研究中,研究人员证实胶质瘤干细胞通过SDF-1/CXCR4信号轴朝着内皮细胞转化,随后在转化生长因子β(TGF-β)作用下诱导生成了周细胞。
这些研究表明,胶质瘤干细胞促使生成了血管周细胞,有可能积极重塑了血管周围微环境。靶向治疗胶质瘤干细胞源性周细胞有可能是有效阻止肿瘤进展,提高抗血管生成治疗效果的一条有潜力的新途径。

DOI:10.1016/j.cell.2013.02.021
PMC:
PMID:
Glioblastoma Stem Cells Generate Vascular Pericytes to Support Vessel Function and Tumor Growth
Lin Cheng, Zhi Huang, Wenchao Zhou, Qiulian Wu, Shannon Donnola, James K. Liu, Xiaoguang Fang, Andrew E. Sloan, Yubin Mao, Justin D. Lathia, Wang Min, Roger E. McLendon, Jeremy N. Rich, Shideng BaoGlioblastomas (GBMs) are highly vascular and lethal brain tumors that display cellular hierarchies containing self-renewing tumorigenic glioma stem cells (GSCs). Because GSCs often reside in perivascular niches and may undergo mesenchymal differentiation, we interrogated GSC potential to generate vascular pericytes. Here, we show that GSCs give rise to pericytes to support vessel function and tumor growth. In vivo cell lineage tracing with constitutive and lineage-specific fluorescent reporters demonstrated that GSCs generate the majority of vascular pericytes. Selective elimination of GSC-derived pericytes disrupts the neovasculature and potently inhibits tumor growth. Analysis of human GBM specimens showed that most pericytes are derived from neoplastic cells. GSCs are recruited toward endothelial cells via the SDF-1/CXCR4 axis and are induced to become pericytes predominantly by transforming growth factor β. Thus, GSCs contribute to vascular pericytes that may actively remodel perivascular niches. Therapeutic targeting of GSC-derived pericytes may effectively block tumor progression and improve antiangiogenic therapy.
(责任编辑:zengchang)
分享到:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#胶质瘤干细胞#
34
#CEL#
18
#Cell#
20
#血管功能#
0