ATVB:巨噬细胞依赖的硫化氢耗竭驱动肥胖患者微血管内皮功能障碍!
2017-03-24 xing.T MedSci原创
由此可见,血管周围脂肪组织诱导型一氧化氮合酶活性-常驻促炎巨噬细胞通过降低血管内H2S的生物利用度促进微血管内皮功能障碍。这些发现支持了一个模型,即肥胖患者中血管H2S耗尽支持血管外周脂肪组织抗收缩功能障碍。
个体发生肥胖时,血管周围脂肪组织作为微血管抗收缩因素的功能出现障碍。肥胖导致炎症和招募炎性巨噬细胞进入到血管周围的脂肪组织,伴随着血管中血管舒张信号分子硫化氢(H2S)的耗尽。近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,研究人员旨在评估巨噬细胞在血管H2S中的作用以及明确如何它影响血管舒张功能。
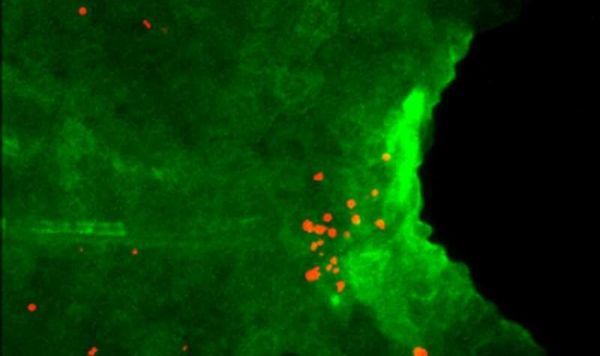
研究人员采用压力肌动描记法和激光共聚焦显微镜分别测定了来自于精瘦和肥胖小鼠肠系膜阻力小动脉的收缩性和H2S水平。
研究人员发现相比于来源于精瘦的对照小鼠,肥胖小鼠的血管舒张受损,平滑肌和血管内皮细胞内的H2S也明显减少。将来自于精瘦老鼠血管与来自于肥胖小鼠的巨噬细胞或巨噬细胞条件培养基共培养,该血管可以重复肥胖表型。这些效应被低分子量的物质所介导,并且依赖于巨噬细胞诱导型一氧化氮合酶活性。
由此可见,血管周围脂肪组织诱导型一氧化氮合酶活性-常驻促炎巨噬细胞通过降低血管内H2S的生物利用度促进微血管内皮功能障碍。这些发现支持了一个模型,即肥胖患者中血管H2S耗尽支持血管外周脂肪组织抗收缩功能障碍。
原始出处:
Joseph Candela,et al. Microvascular Endothelial Dysfunction in Obesity Is Driven by Macrophage-Dependent Hydrogen Sulfide Depletion.ATVB.2017.https://doi.org/10.1161/ATVBAHA.117.309138
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管内皮功能#
43
#内皮功能障碍#
46
#TVB#
34
#肥胖患者#
28
#血管内皮功能障碍#
32
#微血管#
38
#功能障碍#
36
#内皮功能#
38
#硫化氢#
44