Diabetologia:2型糖尿病与听力损失发生率分析
2018-11-19 AlexYang MedSci原创
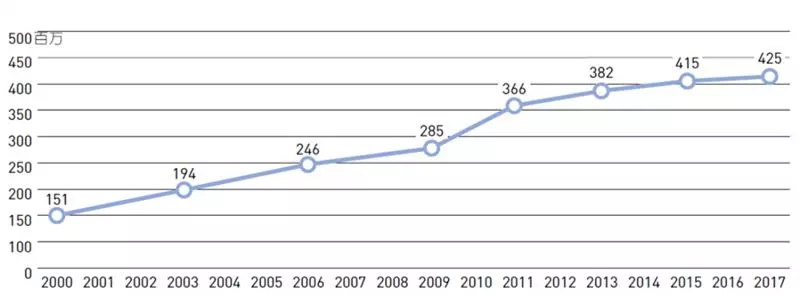
2型糖尿病已经被认为是一种听力损失的风险因子,可能的机制包括微血管疾病、听觉神经病变或者氧化胁迫。虽然有小部分研究调查2型糖尿病与听力损失之间的纵向性关系,但是跟大规模的研究是需要的。最近,有研究人员在2个前瞻性群体中调查了是否2型糖尿病与听力损失的发生率相关。研究人员进行的研究包括了139909名女性,并且调查了2型糖尿病与她们自我报道的听力损失发生之间的相关性,并从2年1次的调查问卷中确定了医
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
36
#发生率#
47
#BET#
29
#听力#
30
谢谢MedSci提供最新的资讯
43