Cell:肠道神经元帮助免疫系统调节肠道炎症
2016-01-25 佚名 生物谷
免疫系统主要负责防御机体可能遭受的感染,因此会始终保持警觉保护机体免受外来威胁,但是免疫系统过度敏感也会造成过度炎症反应并会导致永久性组织损伤,因此保证免疫系统应答的平衡对于机体健康状况的调节非常重要。一项最新研究发现小肠内的神经元细胞能够向免疫细胞发送信号,在保护小肠组织免受过度炎症损伤方面发挥重要作用。 相关研究结果发表在国际学术期刊cell上,这项发现对于肠易激综合征等胃肠道疾病的

免疫系统主要负责防御机体可能遭受的感染,因此会始终保持警觉保护机体免受外来威胁,但是免疫系统过度敏感也会造成过度炎症反应并会导致永久性组织损伤,因此保证免疫系统应答的平衡对于机体健康状况的调节非常重要。一项最新研究发现小肠内的神经元细胞能够向免疫细胞发送信号,在保护小肠组织免受过度炎症损伤方面发挥重要作用。
相关研究结果发表在国际学术期刊cell上,这项发现对于肠易激综合征等胃肠道疾病的治疗具有重要提示意义。
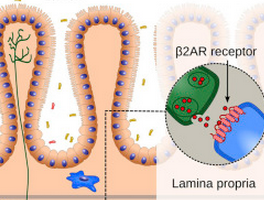
小肠组织中存在着许多类型的免疫细胞,其中包括巨噬细胞,但巨噬细胞也存在不同的群体。固有层巨噬细胞是非常靠近小肠壁的一群细胞,而肌层巨噬细胞则位于小肠组织的更深层部位,距离穿过小肠的物质相对较远。
在这项研究中研究人员利用一种能够展现细胞三维结构形态的成像技术直接观察了上述两群巨噬细胞之间存在的差别,结果发现这两群细胞除了在形态和细胞运动方面存在一定差异,研究人员还注意到这些巨噬细胞在小肠神经元周围的分布也存在差异。
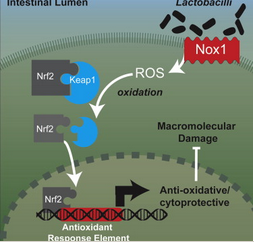
随后研究人员对这两群巨噬细胞的基因表达进行了分析,发现固有层巨噬细胞倾向于表达促炎症基因,与之相比,肌层巨噬细胞倾向于表达抗炎症基因,并且在小肠感染发生之后肌层巨噬细胞的抗炎基因表达也会得到增强。
于是研究人员提出一个问题,肌层巨噬细胞对感染产生快速应答的信号来自于哪里?经过研究之后他们得出结论,其中一部分信号可能来自于肌层巨噬细胞围绕的神经元。
肠脑轴如何阻止炎症?
在另外一些实验中,研究人员发现肌层巨噬细胞携带了一些细胞表面受体,帮助它们应答神经元产生的去甲肾上腺素信号。研究人员认为这种受体的出现可能是神经信号调节免疫细胞进而阻止炎症反应的一种新机制。
他们还发现肌层巨噬细胞会在感染发生后一到两小时内发生激活,这一应答速度明显快于完全依赖免疫系统的应答过程,因此研究人员表示这些位于小肠深层组织内的巨噬细胞接收了神经元产生的信号,即使没有直接接触到病原体也能够对感染产生快速应答。
这项研究对于小肠神经元与巨噬细胞之间的信号交流进行了深入探讨,同时提示在一些严重的肠道感染过程中,这种交流机制可能得到了阻碍,进而导致了组织损伤以及胃肠道疾病的发生。因此这项研究对于炎症导致的胃肠道疾病治疗具有重要提示意义。
原始出处:
Ilana Gabanyi,Paul A. Muller1,et al,Neuro-immune Interactions Drive Tissue Programming in Intestinal Macrophages.cell.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,谢谢作者分享!
90
#CEL#
38
#Cell#
32
也是醉了
163
也许是真的了
136
#肠道炎症#
50
经典
152
上一楼牛
144
这篇文章很有深度,是一篇不错的文章
78