Nat Methods:高端成像技术让癌细胞无所遁形
2015-11-12 佚名 生物谷
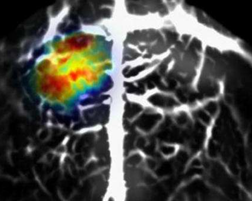
图片来源:medicalxpress.com 利用高科技的成像方法,来自华盛顿大学的科学家就可以在组织深处清楚地看到早期发育中的癌细胞,这或许比之前利用荧光蛋白来观察癌细胞要更加清晰直观,相关研究发表于国际杂志Nature Methods上。 研究者Lihong Wang表示,通过遗传性地修饰胶质母细胞瘤细胞使其表达BphP1蛋白,我们就可以利用光声层析成像 (Photoacoustic

图片来源:medicalxpress.com
利用高科技的成像方法,来自华盛顿大学的科学家就可以在组织深处清楚地看到早期发育中的癌细胞,这或许比之前利用荧光蛋白来观察癌细胞要更加清晰直观,相关研究发表于国际杂志Nature Methods上。
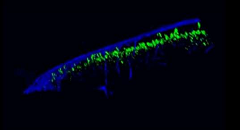
研究者Lihong Wang表示,通过遗传性地修饰胶质母细胞瘤细胞使其表达BphP1蛋白,我们就可以利用光声层析成像 (Photoacoustic tomography)在组织1厘米深处清楚地观测成百上千个活的癌细胞,光声层析成像技术是一种新型的无损无创生物医学影象技术;本文研究工作中研究人员首次将深度侵入技术、高分辨率的光声成像技术同可逆转的可变开关非荧光的细菌光敏色素相结合进行研究。
研究者指出,蛋白质的遗传编码可以使得我们对组织深处的生物学过程进行成像并且靶向追踪,而蛋白质的光控开关特性也可用作新的成像功能;BphP1蛋白可以感知不用类型的光,同时相应改变其吸收特性,这种特性就可以帮助研究者利用两种类型的光:红光或近红外光来获取癌性组织的成像结果,同时也可以对成像结果进行对比来获取癌细胞高度敏感性及高分辨率的成像结果。
利用光声层析成像技术,研究人员首先在近红外光的帮助下揭示了癌性组织中所表达的特殊蛋白,使其改变了吸收特性,随后研究者利用红光照射癌性组织,即扳动蛋白开关以便其可以回归至原始状态。当减去二次成像后血液信号和其它未知的成像背景就会被消除,以便研究者可以更加清晰地观察癌细胞的存在及其转移过程。
研究者Yao指出,本文研究中所开发的新技术对于癌症成像非常有用,当我们首次观看到早期癌症发生时,癌症组织和健康组织并无差异,因为丰富的血液会给予其足够强的信号,使得癌细胞不会凸显出来,如今利用这种新技术研究者就可以在癌症规模很小的时候就对其进行观察研究。
此前研究中仅可以在组织中观看到相对晚期的癌症细胞,因为来自血液较强的背景信号会遮挡癌细胞,而本文中研究人员所开发的新技术不仅可以帮助进行癌症研究,同时还可以用于心脏组织和癌症免疫疗法的研究,新型技术的开发为生物学家们提供了一种新型的工具来进行癌症遗传特异性的高分辨率及深度成像研究,同时也将助力癌症新型药物的研发。
原文出处:
Junjie Yao, Andrii A Kaberniuk,et al.Multiscale photoacoustic tomography using reversibly switchable bacterial phytochrome as a near-infrared photochromic probe.Nat Methods.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
28
#MET#
30
新技术
121
#癌细胞#
35
#成像技术#
34
新技术
112