J Urol:开放式根治性膀胱切除术与机器人辅助根治性膀胱切除术的早期结果比较
2022-02-11 AlexYang MedSci原创
调查并报告了ORC和RARC(均伴随完全体外(i)UD)的围手术期和6个月(mo)的比较结果。
根治性膀胱切除术(RC)伴尿路改道(UD)仍是一种复杂的手术,具有较高的发病率。尽管机器人辅助膀胱切除术(RARC)的使用正在迅速增加,但开放式膀胱切除术(ORC)仍是治疗的参考选择。到目前为止,所有可用的RCT都是以体外循环的方式进行UD,削弱了完全微创手术的潜在好处。

近期,来自意大利的研究人员在《J Urol》上发表文章,他们调查并报告了ORC和RARC(均伴随完全体外(i)UD)的围手术期和6个月(mo)的比较结果。

研究的参与者中,凡是诊断为cT2-4、cN0、cM0或复发的高等级非肌层浸润性膀胱癌的TURBt患者,以及没有机器人手术麻醉禁忌症的患者,均有资格参与随机化。研究人员根据以下变量,并采用共变数自适应随机化程序对患者进行登记。这些变量包括BMI、ASA评分、基线血红蛋白、计划的UD、新辅助化疗和cT阶段。主要终点是证明RARC伴i-UD在减少50%输血率方面的优越性。
在2018年1月-2020年9月期间,有274名患者计划进行RC;其中96人因姑息性意图而排除。在进行资格评估的178名患者中,有62人拒绝随机化,因此最终有116名连续的患者入选(58名RARC,58名ORC),入选率为65%。6个月后,2名患者失去了随访(无法联系),每个队列各有1名,对结果的影响可以忽略不计。围手术期的并发症、住院时间在各组之间基本上相当。在6个月的随访中,有106名患者接受了HRQoL评估(RARC 52人vs ORC 54人)。
总的来说,两个队列在身体功能、角色功能、疲劳、便秘、腹胀和胀气、身体形象和性功能方面都出现了明显的恶化。接受ORC的病人更有可能出现呼吸困难、食欲不振、腹泻和泌尿系统症状和问题;而接受RARC病人的未来前景也明显恶化。尽管如此,在GLMER分析中,手术方法对所有HR-QoL领域的影响可以忽略不计。在主要终点中,RARC队列的围手术期总输血率明显降低(RARC:22% vs ORC:41%;P=0.046)。

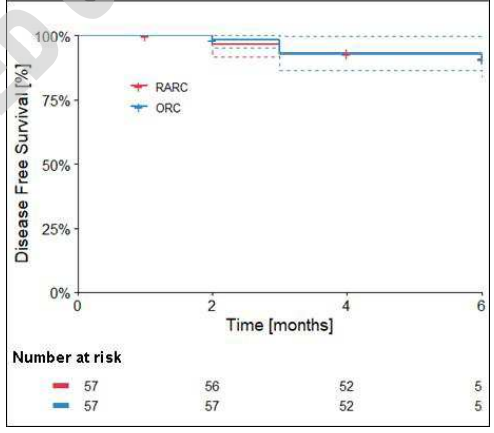
生存结果的Kaplan-Meier曲线
综上所述,该前瞻性随机试验观察到RARC和ORC治疗的患者围手术期总输血率分别为22%和41%,证实了RARC伴i-UD的显著优势。肿瘤学和功能结果需在更长时间的随访中进行评估,以观察各组之间的潜在差异。
原始出处:
Riccardo Mastroianni , Mariaconsiglia Ferriero , Gabriele Tuderti et al. Open Radical Cystectomy Versus Robot-Assisted Radical Cystectomy with Intracorporeal Urinary Diversion: Early Outcomes of a Single Center Randomised Controlled Trial. J Urol. Feb 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#根治性膀胱切除术#
41
#切除术#
33
#机器人#
56
#膀胱切除术#
53
#机器人辅助#
67
#机器#
39
#根治#
36
厉害👍
54