宫颈黑色素瘤一例
2015-12-15 唐良萏教授 中国宫颈疾病网
重庆医科大学附属第一医院 唐良萏教授 整理 病例资料 胡××,67岁,2011.2.21入院。 1. 主诉:绝经20+年,不规则阴道流血2+月 2. 现病史:患者67岁,40+岁绝经(具体不详),绝经后无异常阴道流血、流液及性交出血等。2+月前无明显诱因出现阴道流血,量少,呈暗红色,有臭味,伴轻微下腹部及腰背部胀痛,胀痛持续5天消失,未予重视,
重庆医科大学附属第一医院 唐良萏教授 整理
病例资料
胡××,67岁,2011.2.21入院。
1. 主诉:绝经20+年,不规则阴道流血2+月
2. 现病史:患者67岁,40+岁绝经(具体不详),绝经后无异常阴道流血、流液及性交出血等。2+月前无明显诱因出现阴道流血,量少,呈暗红色,有臭味,伴轻微下腹部及腰背部胀痛,胀痛持续5天消失,未予重视,也未就医。后因持续阴道流血,于入院前10天到当地医院就诊,行宫颈活检后病理提示“宫颈黑色素瘤”,建议其到上级医院就诊。患者遂来我院,经病理复片与外院结果相同,以宫颈黑色素瘤收入院。
3. 既往史及婚育史:既往体健,无手术外伤史。20岁结婚,G6P5,均为顺产。绝经后无阴道流血史,无激素治疗史。无特殊家族病史及遗传病史,无血液系统病史。
4. 专科查体:
外阴:已婚已产式,萎缩
阴道:通畅,见少量淡红色血性分泌物,穹窿浅,肉眼未见浸润
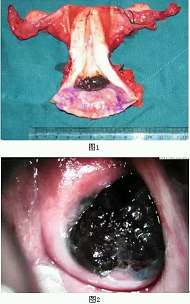
宫颈:萎缩,其上见2*1*1cm大小黑色新生物,外生状,边界清楚,无接触性出血,质偏软
宫体:中位,稍小,活动
两侧:未扪及明显异常
5. 辅助检查:
妇科B超:子宫前位,大小69mm×53mm×37mm,形态尚规则,肌层回声欠均匀,内膜显示欠清,厚4mm。CDFI显示基层内未见异常信号。双卵巢未满意探及。
血常规:白细胞 5.15×109/L,红细胞 3.98×1012/L,血红蛋白 120 g/L,血小板 202×109/L。
凝血象:正常
肝功:总蛋白TP 70g/L,白蛋白ALB 42g/L,ALT 13U/L,AST 18U/L。
肾功:尿素 5.2mmol/L,肌酐 44μmol/L,尿酸 254.4μmol/L。
电解质:钾 3.9 mmol/L,钠145 mmol/L,氯107 mmol/L。
肿瘤指标:CA15-3 7.65 u/ml;CEA 1.48 ng/ml;CA125 <1 u/ml。
空腹血糖:5.09 mmol/L
盆腹腔CT:子宫颈部偏左后增厚呈结节状,最大层面约2.5*2.8cm。平扫CT值为41HU,动脉期为69HU,静脉期为78HU,延迟后为80HU,呈持续中度强化,其内见点状高密度影。符合宫颈肿瘤性病变表现,前方与膀胱左后壁分界欠清,盆腔内未见明显肿大淋巴结影。
TCT:可疑黑色素瘤,建议阴道镜下取活检。
HPV高危型:18型阳性。
阴道镜:原始鳞状上皮,菜花。镜下拟诊:宫颈黑色素瘤。
病理复核:宫颈恶性黑色素瘤
6. 诊断:宫颈黑色素瘤IB1期
7. 治疗: 2011年2月24日在全麻下行经腹广泛全子宫切除+双侧附件切除+盆腔淋巴结清扫术。术中见:腹壁、肠区、大网膜表面未见明显异常,子宫略小,活动,表面光滑,双侧输卵管卵巢未见明显异常。术毕剖视标本:子宫萎缩,宫腔光滑,内膜厚约0.2cm,宫颈管外口见大小约2*1*1cm黑色病灶,侵及肌层外1/3。双输卵管卵巢外观正常,盆腔淋巴结未见明显肿大。
术后病检报告:宫颈恶性黑色素瘤,侵及宫颈壁外1/3。颈管未见累及。阴道残端未见累及。<左髂外、右髂外、左髂总、右髂总、右腹股沟深、左腹股沟深、左闭孔、右闭孔>淋巴结未见癌转移(分别为0/7、0/1、0/3、0/2、0/2、0/2、0/11、0/8)。左、右宫旁未见累及。
术后住院期间予以TP方案化疗一疗程,建议继续补充治疗。
8. 结局:患者自出院后一直未遵医嘱继续随访治疗。时感消化道不适,偶在当地诊所输液。电话随访,患者于术后4年开始出现阴道流液,持续3+月,患者未再入院治疗,于术后4年零3月死亡(71岁)。
9. 诊疗体会:恶性黑色素瘤恶性程度高,女性生殖道的恶性黑色素瘤非常罕见,在女性的各个年龄段均可发生,其发生率仅为恶性黑色素瘤的2%。而大多数的女性生殖道恶性黑色素瘤发生在外阴(76.7%),发生在宫颈的占3-9%。其临床症状与宫颈癌类似,如:异常阴道出血、性交出血等。诊断主要依靠妇科检查、阴道镜以及病理学检查等,少数患者可在常规妇科检查中发现。因此仍可通过定期的宫颈癌筛查早期发现该疾病。治疗上早期者仍以手术为主,辅以放化疗等。晚期则以姑息性治疗为主。
【专家点评】
郑州大学第一附属医院 史惠蓉教授
恶性黑色素瘤可发生于全身许多器官及组织,如口腔、食管、肛管、阴道黏膜等,以皮肤最常见。据报道女性发生在生殖道者仅为3%~7%,以外阴、阴道常见,而发生在宫颈者仅占生殖道恶性黑色素瘤的3%~9%,是罕见的、恶性程度高且预后差的肿瘤。国内仅有散在病例报道。现将该疾病特点总结如下:
一、发病因素
恶性黑色素瘤病因学尚未完全阐明。一些研究资料提示,其发生与基因、环境及基因/环境共同因素有关。另有研究显示免疫抑制或免疫缺陷是恶性黑色素瘤发病的相关因素。该患者HPV 18型阳性,宫颈恶性黑色素瘤是否与HPV感染有关尚未定论。
二、诊断
1. 临床表现:宫颈恶性黑色素瘤好发于围绝经期妇女,临床多呈息肉状、乳头状、菜花状或结节状,棕黑色或蓝黑色肿物突起在宫颈外口,有时呈溃疡状。临床上与宫颈癌无法区别。
2. 影像学检查首选MRI:与CT相比,MRI的优点是对软组织的分辨率高,并能够进行轴位、矢状位、冠状位的多层面、多方位扫描,可以更清楚地显示宫颈与周围组织的关系。MRI中宫颈癌灶在T2加权像上表现为破坏间质(低信号)的高信号团块,该特点使MRI对诊断宫颈癌灶与宫旁浸润的准确率更高。有文献报道,由于黑色素是顺磁性物质,故其MRI表现具有特异性,即恶性黑色素瘤的原发肿瘤和转移瘤在T1WI像均呈高信号,据此可以提高诊断宫颈恶性黑色素瘤的敏感性。因宫颈恶性黑色素瘤极为罕见,相关资料匮乏,故该结论尚需更多的病例证实。
3. 病理诊断:恶性黑色素瘤以镜下表现千变万化而著称,其特点是细胞形态和组织结构的多样性。瘤细胞可含丰富色素、少量色素或无色素。对少色素或无色素性恶性黑色素瘤的诊断较为困难,在作出病理诊断时要与癌( 鳞癌、腺癌、未分化癌)、肉瘤、癌肉瘤、淋巴瘤和绒癌鉴别,除了观察HE切片外,常需借免疫组化染色方法协助确诊。
三、鉴别诊断
需与病理诊断相结合与以下疾病鉴别:(1)首先应排除宫颈转移性恶性黑色素瘤;(2)宫颈鳞状细胞癌;(3)宫颈神经内分泌肿瘤;(4)宫颈蓝痣。
四、治疗
1. 手术为主:广泛子宫切除+盆腔淋巴结清扫,阴道侵犯时需同时行阴道全切术及腹股沟淋巴结清扫。由于宫颈恶性黑色素瘤的病例数少,目前尚无大样本的前瞻性临床研究结果证实淋巴结清扫的意义。腹主动脉旁淋巴结清扫的意义更是鲜有文献报道。
2. 放疗:主要用于不能手术者或术后切缘阳性患者。
3. 化疗:氮烯咪胺(DTIC)是单药治疗黑色素瘤有效的药物,其与口服制剂替莫唑胺的有效率均为12%~20%。目前NCCN推荐用于黑色素瘤治疗的化疗方案包括DTIC或替莫唑胺单药治疗、CVD方案(DTIC+DDP+长春碱类)及紫杉醇单药治疗或TP方案(紫杉醇联合铂类)。
4. 由于免疫抑制或免疫缺陷是恶性黑色素瘤发病的相关因素,因此,使用免疫抑制剂可作为治疗宫颈恶性黑色素瘤的一项重要辅助性手段。在黑色素瘤患者中的前瞻性随机临床试验表明,与单纯化疗相比,采用不同化疗方案联合免疫治疗可提高疗效。
5. 目前特异性免疫治疗及靶向治疗的迅速发展为宫颈及阴道恶性黑色素瘤的治疗提供了新的治疗手段。伊匹单抗、维罗非尼、伊马替尼在治疗晚期黑色素瘤中均有文献报道,值得在阴道及宫颈恶性黑色素瘤中进一步研究。
五、预后
研究表明,恶性黑色素瘤患者因原发部位的不同,其预后存在较大差异。外阴恶性黑色素瘤5 年生存率为30%~50%,而阴道恶性黑色素瘤仅为14.5%~21%。宫颈恶性黑色素瘤由于发病率极低,尚无5年生存率的报道,可能更差。
影响预后的因素:文献报道提示,肿瘤<3 cm的患者预后较好,脉管癌栓患者中位OS明显低于无脉管癌栓患者。盆腔淋巴结转移患者中位PFS显著低于无转移患者。而年龄、肿瘤部位、有无色素沉着、有无肿瘤家族史、FIGO分期、手术方式、区域淋巴结清扫、肌层浸润深度、切缘等因素未发现与PFS或OS显著相关。
该病例是临床表现典型的宫颈恶性黑色素瘤,其诊断、分期均明确,手术行广泛子宫切除+双附件切除+盆腔淋巴结清扫术,范围足够。宫颈恶性黑色素瘤本身恶性程度极高、预后极差,患者术后未完成全部化疗疗程仍生存4年零3个月实属不易。
关于该例宫颈恶性黑色素瘤的诊断和治疗,仅有以下建议供参考。
1. 根据文献报道,恶性黑色素瘤的MRI表现有其特异性,无论是原发肿瘤或转移瘤在T1WI像均呈高信号,同时MRI能够进行轴位、矢状位、冠状位的多层面、多方位扫描,有助于提高诊断的敏感性和准确性,故该类病例的影像学检查建议首选MRI(除非患者有MRI检查禁忌)。
2. DTIC是首先被FDA批准应用于治疗恶性黑色素瘤的药物,所以宫颈恶性黑色素瘤术后化疗选用DTIC为一线用药可能更为合适。因DTIC药源不足,临床上也可选用紫杉醇联合铂类的化疗方案作为辅助治疗。免疫治疗在恶性黑色素瘤治疗中具有重要作用,如果患者有条件,可在化疗同时加用免疫治疗,有助于提高患者的预后。
【专家点评】
中国医科大学附属盛京医院 张淑兰教授
宫颈恶性黑色素瘤在临床上极为罕见,好发于围绝经期妇女。恶性黑色素瘤是起源于上皮基底层黑色素细胞的恶性肿瘤,女性生殖道恶性黑色素瘤发生率为恶性黑色素瘤的2%,主要发生在外阴及阴道。
宫颈恶性黑色素瘤的常见临床表现为不规则阴道流血、绝经后出血及阴道分泌物增多。妇科检查常见宫颈外口息肉状、乳头状、菜花状或结节状黑色或黑蓝色肿物,大小从几毫米到几厘米不等,触之无出血,表面可伴有溃疡,可向临近宫颈或阴道侵袭。病理组织检查是诊断宫颈恶性黑色素瘤的金标准。
目前宫颈黑色素瘤尚缺乏统一的治疗标准。手术治疗是宫颈恶性黑色素瘤的首选治疗方法。国内外学者多采用广泛全子宫切除术,包括2cm以上阴道安全切缘,联合盆腔淋巴结清扫,累及阴道者应行全部或部分阴道切除术,是否行淋巴结清扫尚仍存在争议。在黑色素瘤的综合治疗中,化疗是重要的辅助治疗方法之一。氮烯咪胺(DTIC)是唯一被美国食品和药物管理局(FDA)批准为治疗恶性黑色素瘤的药物,有效率为20%。放疗对宫颈黑色素瘤效果不佳。免疫治疗是 恶性黑色素的有效治疗手段之一,γ-干扰素的应用使得本病的生存率明显提高。宫颈恶性黑色素瘤和其他部位一样,恶性程度高,预后差,5年生存率仅为7.41%。肿瘤大小、浸润深度及淋巴结转移是影响预后的主要因素。早期的诊断及根治性手术可能延长患者生存时间,改善生存质量。开展宫颈癌普查是发现早期病例的简单易行的方法。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#色素#
24
第一次见
101
首次见
92
#宫颈#
21
#黑色素#
25
#黑色素#
31