《国家医保药品目录》落地:优化ASCVD患者的降脂方案,阿利西尤单抗直接医保应用
2022-01-02 梅斯医学 梅斯医学
降低LDL-C水平,预防ASCVD发生发展。
2022年1月1日,新版《国家医保药品目录(2021年)》开始正式执行,其中就包括了创新型降脂药PCSK9抑制剂阿利西尤单抗注射液(波立达®),这也意味着将有更多动脉粥样硬化性心血管疾病(ASCVD)患者,可以更便捷地获得阿利西尤单抗注射液(波立达®)进行降脂治疗。新版《国家医保药品目录(2021年)》的落地实施,对ASCVD患者的降脂治疗必将会带来更多积极且深远的影响。
降低LDL-C水平,预防ASCVD发生发展
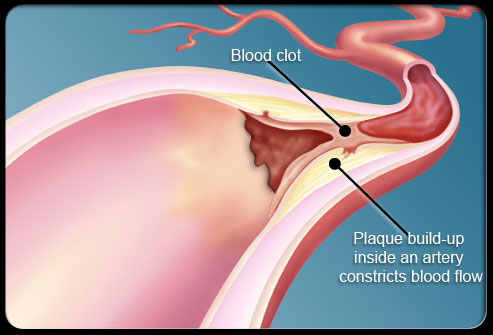
近年来,随着社会老龄化和城市化进程加快,不健康生活方式的流行,我国居民动脉粥样硬化性心血管疾病(ASCVD)发生率持续攀升。当前,ASCVD死亡已成为我国居民第一位的死亡原因[1],而血脂异常则是ASCVD发生发展中最重要的一个致病性危险因素,据《中国心血管健康与疾病报告2020》[2]显示,每5个死亡患者中就有2个是心血管疾病。因此,有效控制血脂异常,对我国ASCVD的防控具有非常重要的意义。对于ASCVD患者的血脂管理,无论循证研究还是临床实践均已证实[3],对于低密度脂蛋白胆固醇(LDL-C)水平的良好控制可以改善ASCVD患者的预后,降低心血管不良事件发生率。权威指南[4-6]亦指出,降低LDL-C水平,能够预防动脉粥样硬化性心血管疾病(ASCVD)进一步发生发展。
循证证据支持,PCSK9抑制剂降脂快速且安全
针对ASCVD患者的LDL-C治疗目标,《2019欧洲心脏病学会/欧洲动脉粥样硬化学会(ESC/EAS)血脂异常管理指南》[4]建议,高危患者的LDL-C目标为<1.8 mmol/L(<70 mg/dL),且比基线降低至少50%;极高危患者的LDL-C目标为<1.4 mmol/L(<55 mg/dL)且比基线降低至少50%;如果ASCVD患者接受最大耐受剂量他汀治疗后2年内发生第二次事件,则考虑将LDL-C降至<1.0 mmol/L(<40 mg/dL)。北京大学第一医院霍勇教授认为,虽然多年来,大家一直强调控制血脂的重要性,但是临床实践中,对于高危/极高危ASCVD或是做过PCI治疗的患者而言,即便是谨遵医嘱用药,仍有很多患者的LDL-C控制难以达标。近年来,随着PCSK9抑制剂在中国的上市应用,已经有越多越多抗动脉粥样硬化不理想的ASCVD患者获得了理想的治疗。ODYSSEY OUTCOMES研究证实,在大量他汀的使用基础上,PCSK9抑制剂阿利西尤单抗仍能进一步降低LDL-C,12个月LDL-C降幅高达61%,达标率高达94.6%,可显著降低主要不良心血管事件(MACE)15%,并与全因死亡风险下降相关。这也是目前唯一被证实与全因死亡下降相关的PCSK9抑制剂。ODYSSEY EAST研究显示:持续使用PCSK9抑制剂阿利西尤单抗4周,可以快速强效降低LDL-C至指南推荐目标水平。为此,霍勇教授特别强调,对于合并冠状动脉多支血管病变、发生多次冠脉事件、糖尿病、多血管床病变等高危因素的ASCVD人群,建议应用PCSK9抑制剂,如阿利西尤单抗进行强化降脂治疗。
应用方式更便捷,PCSK9抑制剂降脂疗效不打折
随着新版《国家医保药品目录(2021年)》的落地实施,患者对于PCSK9抑制剂的获取也会更容易,将进一步解决诸多高危/极高危ASCVD患者面临的血脂管理难以达标的难题。《2018美国心脏病学会/美国心脏协会(AHA/ACC)血胆固醇管理指南》[5]强调,PCSK9抑制剂联合他汀类药物可以达到进一步降低LDL-C水平的目的,尤其适合于极高危的ASCVD人群。《2019 ESC/EAS血脂异常管理指南》[4]推荐:对于极高风险患者的二级预防,如果最大耐受剂量他汀和依折麦布治疗后LDL-C仍未达标,推荐联合PCSK9抑制剂。《急性冠脉综合征患者血脂管理临床路径专家共识(2020)》亦建议,对于复发ASCVD患者、合并冠状动脉多支血管病变、糖尿病以及LDL-C≥4.9 mmol/L(190 mg/dl)等合并高风险因素的ACS患者,当既往的治疗方案不足以将LDL-C降至目标水平时,建议可联合使用PCSK9抑制剂进行降脂治疗。正如霍勇教授所强调的,患者才是自身健康的第一责任人,相信PCSK9抑制剂每两周一次皮下注射的方式,一定能够帮助更多ASCVD患者提升用药依从性,助力血脂管理达标,更好地控制动脉粥样硬化性心血管疾病的发生发展。
“健康至上,生命至上”,一直是我国健康事业坚持不变的发展理念。相信随着《国家医保药品目录(2021年)》的施行,两周一次皮下注射的PCSK9抑制剂阿利西尤单抗,在帮助越来越多ASCVD患者获得有效治疗的同时,也能够进一步减轻患者及其家庭经济负担,让更多人拥有更高质量的幸福生活。
参考文献
[1]顾景范. 《中国居民营养与慢性病状况报告(2015)》解读[J]. 营养学报, 2016, 38(6):5.
[2]中国心血管健康与疾病报告2020[J]. 心肺血管病杂志, 2021, 40(9):5.
[3]杨芬, 苏冠华, & 程翔. (2021). 干预低密度脂蛋白胆固醇是动脉粥样硬化性心血管病防治的根本措施. 中华心血管病杂志, 49(6), 5.
[4] Mach F , Baigent C , Catapano A L , et al. 2019 ESC/EAS Guidelines for themanagement of dyslipidaemias: lipid modification to reduce cardiovascular risk[J]. Russian Journal of Cardiology, 2020, 25(5):3826.
[5] Grundy S M , Stone N J , Bailey A L , et al.
2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol[J]. Journal of the American College of Cardiology, 2018, 73(24).
[6]Maurizio Averna, Maciej Banach, Eric Bruckert, et al. Practical guidance for combination lipid-modifying therapy in high- and very-high-risk patients: A statement from a European Atherosclerosis Society Task Force. April 12, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







.jpg)




#医保药品#
41
#ASC#
0
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
64
#ASCVD#
48
坚持学习
74
好消息
54
学习了
60
👍
62