Oncotarget:PTPRO介导的自噬可以阻止脂肪肝和肝细胞癌发生
2015-04-07 沐晴 译 MedSci原创
以往研究表明细胞自噬在非酒精性脂肪肝(NASH)和肝细胞癌(HCC)的进展中起非常重要的作用。蛋白酪氨酸磷酸酶受体O (PTPRO)是最近发现的肿瘤抑制因子,但是关于它在NASH的研究很少。近来有研究,证明PTPRO介导的细胞自噬与胰岛素抵抗、脂代谢、肝癌发生相关。 研究者选取同源的野生型小鼠(对照组)和ptpro−/−小鼠(试验组)作为实验对象,首先使用二乙基亚硝胺造NAS
以往研究表明细胞自噬在非酒精性脂肪肝(NASH)和肝细胞癌(HCC)的进展中起非常重要的作用。蛋白酪氨酸磷酸酶受体O (PTPRO)是最近发现的肿瘤抑制因子,但是关于它在NASH的研究很少。近来有研究,证明PTPRO介导的细胞自噬与胰岛素抵抗、脂代谢、肝癌发生相关。
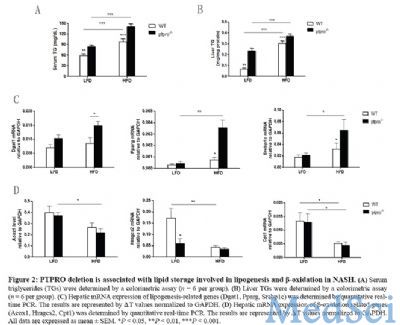
研究者选取同源的野生型小鼠(对照组)和ptpro−/−小鼠(试验组)作为实验对象,首先使用二乙基亚硝胺造NASH小鼠模型,然后分别给予两组小鼠高脂饮食16周。结果显示,与野生型小鼠相比,ptpro−/−小鼠出现了严重的肝损伤、胰岛素抵抗、肝脂肪变性及自噬缺陷。同时,PTPRO基因敲出也促进了脂质生成目标基因的表达,减少了β氧化途径相关基因的活性。此外,发现ptpro−/−小鼠中,AKT的激活增加,胞浆中p53积聚增多,这两种变化一起抑制细胞自噬。有趣地是,由于PTPRO基因敲出,与AKT激活相关的高胰岛素血症在高脂饮食的小鼠中进一步加重了。AKT的激活诱导MDMX/MDM2杂合物的稳定性,从而促进p53在胞浆中积聚。抑制AKT可以修复自噬和肝细胞中p53的积聚,这表明AKT作用于p53的上游基因。由于ptpro−/− 小鼠存在高胰岛素血症和自噬缺陷,高脂饮食可能加重其肝脂肪变性。重要的是,脂肪肝的肝细胞胞浆中PTPRO的表达明显减少与p53积聚增加有关。
最后,研究者认为其之前的研究已经证明与癌旁组织相比,肝细胞癌中PTPRO 的水平显著降低了,而小鼠实验进一步证明,与正常脂质饮食相比,高脂饮食抑制PTPRO的表达,PTPRO 可能通过PI3K/Akt/MDM4/MDM2/P53途径影响肝细胞自噬,进而调节胰岛素和脂质代谢。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,谢谢分享!
53
#细胞癌#
26
#target#
27
#肝细胞#
31
不错,学习了
118
新药的基础课
122
#PRO#
20
支持
107
值得学习
123
很好的资料
133