CHC2018丨贾海波教授:OCT对斑块破裂的判定及临床意义
2018-08-09 国际循环编辑部 国际循环
斑块破裂(plaque rupture)是急性心肌梗死发病的高风险因素之一,光学相干断层成像(OCT)技术可识别斑块特征,指导治疗。近日,在CHC 2018学术大会上,哈尔滨医科大学附属第二医院贾海波教授就相关专题发表精彩报告。
斑块破裂(plaque rupture)是急性心肌梗死发病的高风险因素之一,光学相干断层成像(OCT)技术可识别斑块特征,指导治疗。近日,在CHC 2018学术大会上,哈尔滨医科大学附属第二医院贾海波教授就相关专题发表精彩报告。
急性冠状动脉综合征(acute coronary syndrome,ACS)是冠心病致死的主要类型,OCT因其无可比拟的高分辨率,被认为是目前在体识别ACS重要病理机制——斑块破裂的最佳影像学手段。贾海波教授就OCT对斑块破裂的发生率、影像学判定、临床意义展开阐述。
一、斑块破裂的发生率
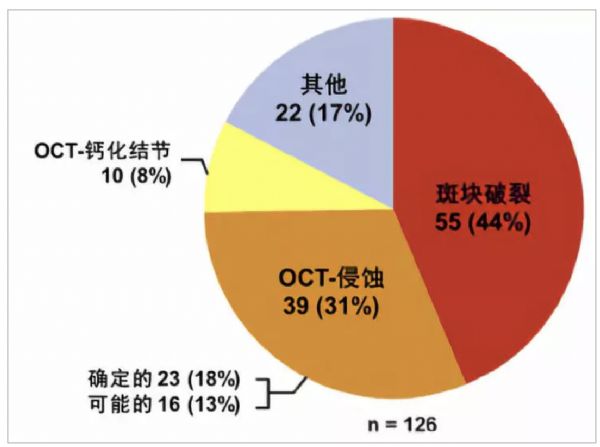
尸检研究发现ACS患者斑块破裂的发生率为50%~75%。一项最新数据显示,约73%的致死性冠状动脉事件由斑块破裂导致。在体研究同样显示,斑块破裂是导致ACS发生的主要原因。近期,哈尔滨医科大学附属第二医院于波教授及团队开展的一项OCT研究,对ACS的罪犯斑块进行了系统分类和定义,发现OCT定义下的斑块破裂、斑块侵蚀及钙化结节分别占ACS罪犯病变的43.7%、31.0%、7.9%(图1)。
图1. ACS患者在体OCT检测的发病机制
在126个罪犯病变中,斑块破裂占44%,斑块侵蚀占31%(可能的斑块侵蚀为13%,确定的斑块侵蚀为18%),钙化结节占8%,其他病变占17%。
二、斑块破裂的定义
目前,一致认为,斑块破裂的定义为脂质斑块的纤维帽连续性中断(disruption),继而使斑块内易引起血栓的核心暴露至血流中[8]。病理上典型的破裂斑块通常含有较大的脂质/坏死核心(>30%斑块面积),薄纤维帽的断裂,并伴有大量巨噬细胞、淋巴细胞浸润,平滑肌细胞一般较少。
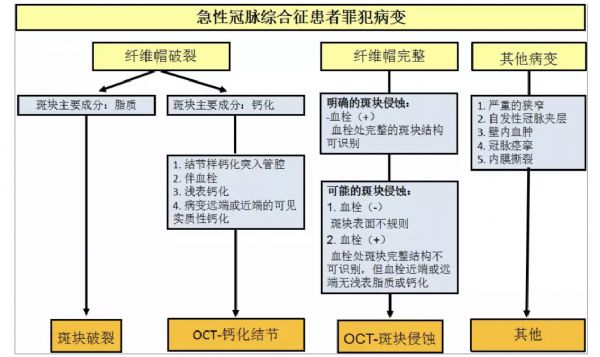
与病理学结果相比,OCT对活体患者斑块破裂的诊断标准没有要求斑块表面有血栓覆盖,因为患者在行OCT成像之前可能已行抗栓或溶栓治疗,故成像时血栓可能减少或完全消失。于波团队的一项OCT研究首次在体详细定义了OCT影像检测的斑块侵蚀和钙化结节,并提出了分类标准,明确指出斑块侵蚀与斑块破裂在临床特征和影像学上均存在显著不同,此项研究对ACS发病机制的在体研究及治疗策略选择具有重要的指导作用(图2)。OCT图像上斑块破裂的定义为:脂质斑块的纤维帽连续性中断,伴空腔形成(图3)。
图2. OCT对ACS罪犯病变的分类和诊断标准
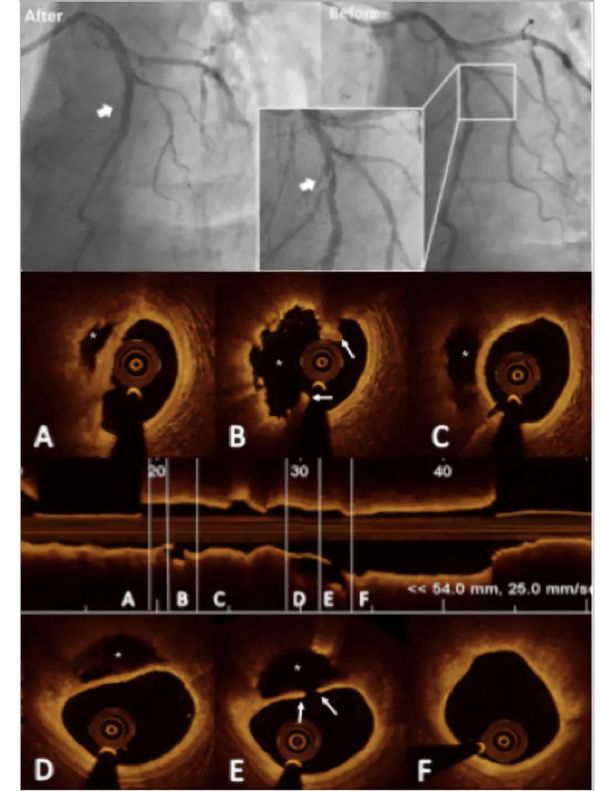
图3. 斑块破裂的典型OCT病例
患者,男,57岁,诊断为ST段抬高型心肌梗死,经溶栓治疗后行OCT成像。(A)冠状动脉造影显示罪犯病变在前降支中段,(B),(C)为OCT图像上的横轴、纵轴切面,斑块破裂表现为纤维帽连续性中断(箭头),斑块内部空腔形成(*)。
三、识别破裂的临床意义
研究发现,纤维帽厚度(<52 μm)是易损斑块破裂的关键决定因子,一项OCT的在体研究也提示FCT是决定斑块不稳定性的重要因素。此外,Ino等人的研究发现,与NSTE-ACS患者相比,STEMI患者斑块破口更大,破口方向多逆向血流方向(46% vs. 17%,P=0.036)。因此,破裂关键影像学特征与临床急性事件的关系仍待进一步研究。
四、典型病例:多发斑块破裂致急性ST段抬高型心肌梗死
患者,男,67岁,主因“阵发性心悸、气短1年余,加重1个月”入院。诊断为急性前壁ST段抬高型心肌梗死。
冠状动脉造影结果提示,前降支近段狭窄达50%,中段狭窄达60%,前降支OCT结果显示,前降支根部和近中段可见多处斑块破裂伴夹层(图4),给予支架后患者恢复良好。
图4. 多发斑块破裂致心肌梗死
冠状动脉造影示,前降支近中段狭窄伴夹层影像。OCT检查显示两处斑块破裂伴血栓和夹层形成。(A)斑块破裂口远端;(B)破裂口处;(C)破裂口近端。(D-F)近端斑块破裂(E)伴夹层(D)形成,破裂近端为脂质斑块。(*为破裂空腔,箭头所示为破裂口)
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#斑块破裂#
44
#OCT#
38
学习了,谢谢分享
66
#斑块#
31
#CHC#
53
了解一下,谢谢分享!
74