Medicine:中国IFG与糖尿病的前瞻性研究(开滦研究)
2017-01-04 赛诺菲医学部 菲糖新动
Medicine(Baltimore)杂志2016年11月发表了一项中国大规模的前瞻性队列研究——开滦研究,旨在评估中国人群的空腹血糖受损(IFG)与糖尿病的患病率和发病率、空腹血糖升高速率以及与这些结局相关的主要可变风险因素。全球流行病学调查预测,随着中国人口的不断增长,以及老龄化、城市化进程加速,在2000-2030年间,中国的糖尿病患病率将翻一番。或许更令人担忧的是,糖尿病前期的患病率预计比
Medicine(Baltimore)杂志2016年11月发表了一项中国大规模的前瞻性队列研究——开滦研究,旨在评估中国人群的空腹血糖受损(IFG)与糖尿病的患病率和发病率、空腹血糖升高速率以及与这些结局相关的主要可变风险因素。
全球流行病学调查预测,随着中国人口的不断增长,以及老龄化、城市化进程加速,在2000-2030年间,中国的糖尿病患病率将翻一番。或许更令人担忧的是,糖尿病前期的患病率预计比糖尿病的患病率高几倍,从而显著地扩大了高危人群的数量。再加上中国肥胖人群的不断增加,更加导致了IFG和糖尿病发病率的灾难性增加。为了更好地识别IFG和糖尿病高危人群,并采取措施阻止其发展,在中国开展大规模的公共卫生倡议活动,以提高对IFG和糖尿病发病率及相关可变风险因素的认识很有必要。
开滦研究是在中国唐山开滦社区进行的一项前瞻性队列研究,共纳入101,510例≥18岁的参与者,分别于2006、2008和2010年期间进行随访。对其中100,279例参与者进行分析。主要分析4年间糖尿病**和IFG*的患病率和发病率,并确定可能导致该人群糖尿病和IFG发生的可变风险因素。
**糖尿病定义为:自我报告的病史、接受胰岛素或任何口服降糖药治疗、空腹血糖≥7mmol/L;
*IFG定义为:空腹血糖水平在5.6-6.9mmol/L之间。
IFG和糖尿病的患病率
2006年、2008年和2010年IFG年龄标准化患病率分别为17.3%、20.7%和22.6%,糖尿病患病率分别为6.6%、7.6%和7.7%。
IFG和糖尿病的发病率
2006-2010年期间,IFG年龄标准化发病率#为62.6/1000人·年(女性51.2/1000人·年,男性73.8/1000人·年,性别差异P<0.001)。糖尿病年龄标准化发病率#为10.0/1000人·年(女性7.8/1000人·年,男性12.1/1000人·年,性别差异P<0.001)。此外,IFG和糖尿病发病率随年龄增加而增加,在年龄≥60岁人群中性别差异消失(P>0.10)。当进一步纳入癌症和心血管疾病人群后,IFG和糖尿病发病率则增加至75.6/1000人·年和13.9/1000人·年。
#考虑到癌症和心血管疾病会影响到当前血糖控制,故研究未将有癌症和心血管疾病史的人群纳入IFG和糖尿病发病率的分析。
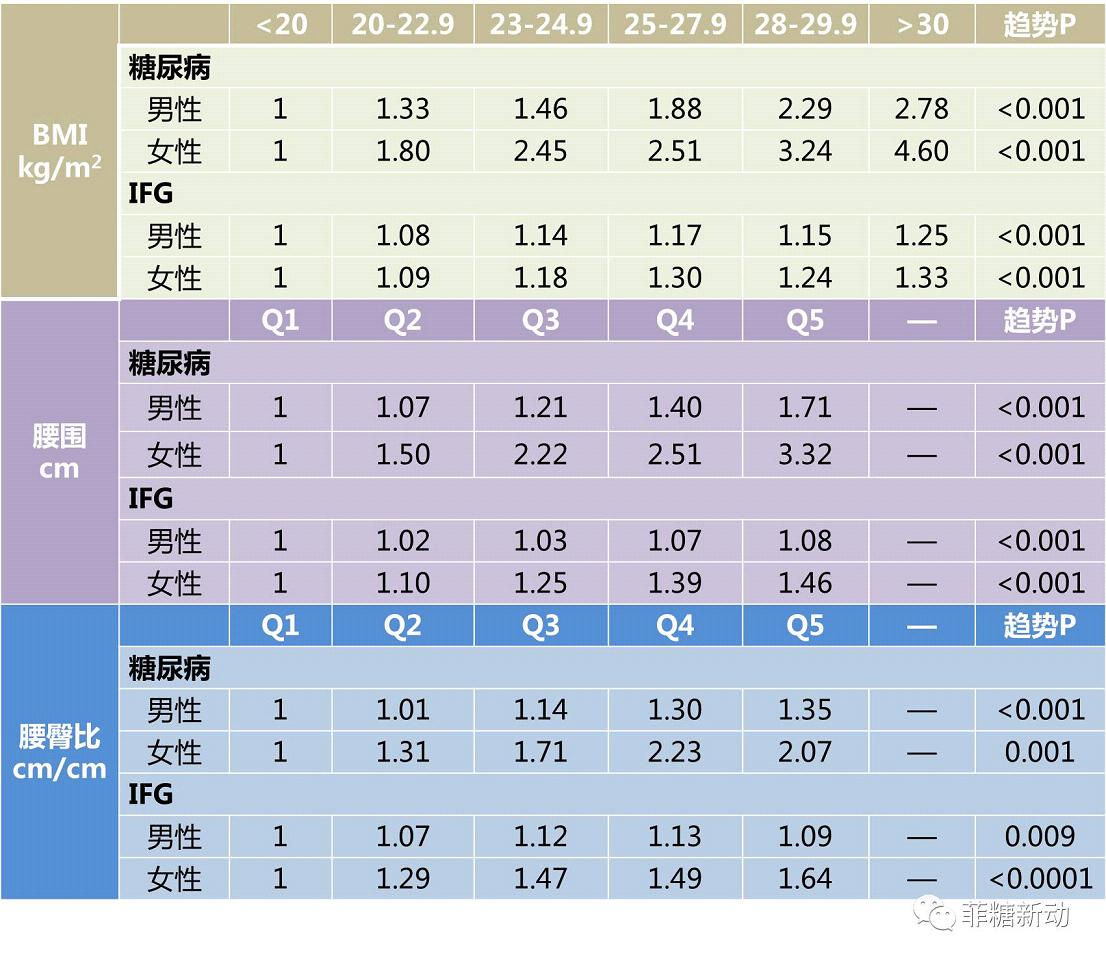
肥胖与糖尿病、IFG风险增加相关
通过BMI、腰围、腰臀比评估肥胖情况。本研究发现:随访4年期间,无论男女,肥胖与糖尿病、IFG风险增加均相关(所有趋势P<0.01)。
肥胖与IFG和糖尿病风险的相关性
每一个BMI分层人群的空腹血糖水平均稳定增加
本研究发现:虽然更高的BMI与血糖水平增加更快有关(男性和女性均P<0.001),但在每一个BMI分层,人群的空腹血糖水平均稳定增加,包括传统认为的BMI在“正常”范围(BMI<23kg/m2)的人群。
随访期间不同BMI分层人群的空腹血糖水平

本研究还进一步观察到: 若同时将BMI和腰围作为预测指标,在非汉族人群中,BMI和腰围越高者,其发展为IFG或糖尿病风险也越高。
综上,在中国成人大型队列中观察到IFG和糖尿病具有高患病率、高发病率,而且在所有体型人群中(即使是较瘦人群),空腹血糖都会稳定增长。通过采取公共政策以加强体育锻炼减轻体重或改善体型,是否可以改善这些不良结局,仍需进一步研究证实。
作者见解本研究是评估中国糖尿病前期和糖尿病发病率及其可变风险因素的最大规模的前瞻性队列研究。对主要可变风险因素的分析将有助于指导公共卫生决策的制定,以减少不良结局的发生。虽然鼓励减重是一种广为接受的改善血糖控制、并最终减少糖尿病发病的干预措施,但对于中国人群来说,可能并不是最理想的方式,因为本研究发现:即使BMI较低,其糖耐量受损风险仍可能增加。另外,单靠BMI这一指标并不能很好地反应体脂分布情况,而腰围可能是更重要的糖尿病发生风险预测指标,尤其是对于BMI较低的人群。总之,有必要通过政策支持以加强健康饮食和身体素质教育,从而优化腰围和BMI水平。
原始出处:
Vaidya A1, Cui L, Sun L, Lu B, Chen S, Liu X, Zhou Y, Liu X, Xie X, Hu FB, Wu S, Gao X.A prospective study of impaired fasting glucose and type 2 diabetes in China: The Kailuan study.Medicine (Baltimore). 2016 Nov
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#前瞻性#
30
#DIC#
33
#前瞻性研究#
45
#开滦研究#
33
#CIN#
26
#Medicine#
30
#Med#
27