Clin Cancer Res:抗集落刺激因子单克隆抗体Lacnotuzumab联合吉西他滨-卡铂治疗三阴性乳腺癌的疗效
2021-10-12 Nebula MedSci原创
吉西他滨-卡铂+拉妥珠单抗治疗方案显著出与吉西他滨-卡铂方案相当的抗肿瘤活性
三阴性乳腺癌(TNBC)约占所有乳腺癌的15%~20%。根据美国临床肿瘤协会/美国学院病理学家指南,TNBC定义:通过免疫组化检测雌激素受体 (ER) 和孕激素受体 (PgR) 表达≤1%。根据免疫组化,HER2水平为0~1或2+。与其他类型的乳腺癌相比,TNBC通常更容易转移,侵袭性更高。
本研究一项II期临床试验,旨在明确在TNBC患者的吉西他滨+卡铂方案中加入拉妥珠单抗(Lacnotuzumab,一种抗集落刺激因子单克隆抗体)的疗效。
招募了肿瘤相关巨噬细胞水平高、不适合手术或放疗的晚期TNBC女性患者,随机分成两组,接受吉西他滨-卡铂+拉妥珠单抗(10 mg/kg·3周)或吉西他滨-卡铂治疗。持续治疗直到出现不可耐受的毒性、疾病进展或医生/患者决定终止治疗。
共招募了49位患者,其中34位接受吉西他滨-卡铂+拉妥珠单抗治疗,15位接受吉西他滨-卡铂治疗。由于治疗领域的快速发展,招募工作面临挑战,最终停止了招募;因此,未对主要终点进行正式的假设检验。
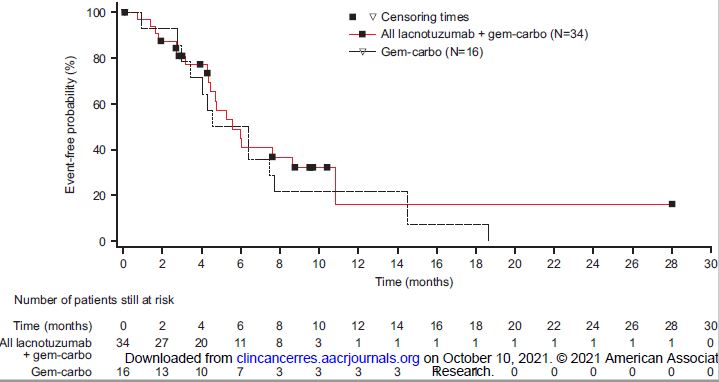
两组的无事件生存率
吉西他滨-卡铂+拉妥珠单抗组和吉西他滨-卡铂组的中位无进展生存期分别是5.6个月(95% CI 4.47-8.64)和5.5个月(3.45-7.46)。
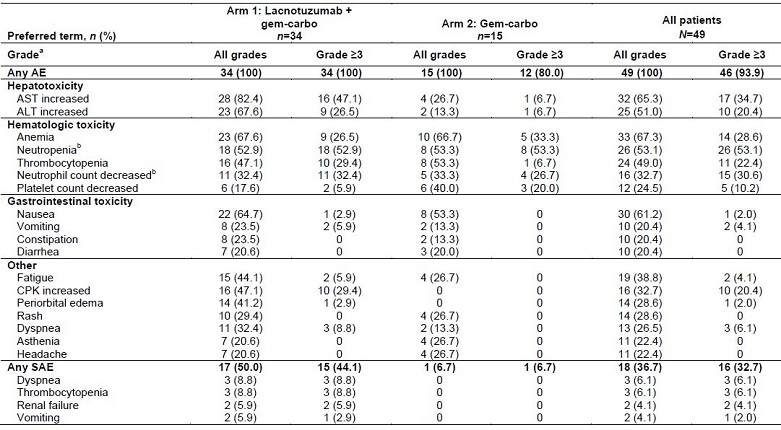
不良事件发生情况
两组均常见血液学不良事件;但是,接受拉妥珠单抗治疗的患者更经常发生天门冬氨酸转氨酶、丙氨酸转氨酶和肌酸激酶升高。
综上所述,吉西他滨-卡铂+拉妥珠单抗治疗方案显著出与吉西他滨-卡铂方案相当的抗肿瘤活性,但耐受性略差。但是,该研究结果为进一步研究靶向集落刺激因子因子在治疗TNBC中的应用提供了信息。
原始出处:
Sherko Kuemmel, et al. A Randomized Phase II Study of Anti-CSF-1 Monoclonal Antibody Lacnotuzumab (MCS110) Combined with Gemcitabine and Carboplatin in Advanced Triple Negative Breast Cancer. Clin Cancer Res October 6 2021 DOI:10.1158/1078-0432.CCR-20-3955
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#铂#
36
#阴性乳腺癌#
0
#克隆#
39
#mAb#
30
#卡铂#
0
#三阴性#
28
学习学习
58
感谢分享
63
学习了
60