NEJM:甲状腺肿患者的Pemberton征-病例报道
2018-05-31 xing.T MedSci原创
Pemberton征出现提示胸腔入口阻塞而引起的上腔静脉综合征。
患者为一名77岁的男子,转诊至内分泌科就亚临床甲状腺功能亢进症进行评估。他没有甲状腺毒症的症状,也没有提示气管受压的呼吸困难或发音障碍症状。
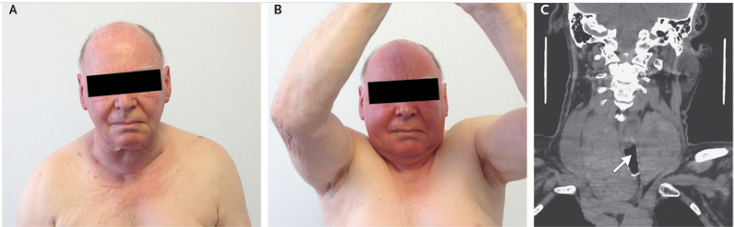
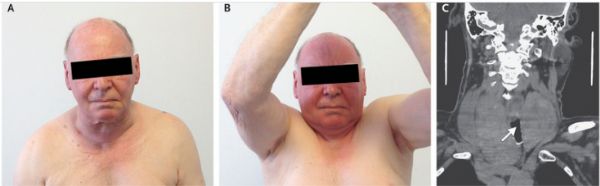
体格检查显示甲状腺肿大,无明显结节或颈部淋巴结肿大(如图A所示)。可以明显观察到Pemberton征-双臂抬高后出现可逆的面部挤塞(如图B所示)。血浆促甲状腺激素水平为0.2mIU/L(参考范围为0.4至4.4),并且血清游离甲状腺素水平正常。颈部计算机断层扫描显示甲状腺肿大,压迫锁骨下静脉和颈静脉(如图C所示),气管偏向左侧(如图C箭头所示)。
Pemberton征出现提示胸腔入口阻塞而引起的上腔静脉综合征。
该患者接受了简单的全甲状腺切除术,病理分析中观察到良性甲状腺肿。他接受了甲状腺激素治疗,手术后6个月随访时,患者甲状腺功能正常。
原始出处:
Yazan Abu-Shama,et al.Pemberton’s Sign in a Patient with a Goiter.N Engl J Med 2018. https://www.nejm.org/doi/full/10.1056/NEJMicm1712263
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#甲状腺肿#
48
#PE#
49
学习
67
谢谢分享.学习了
66
学习了很有用不错
64