骨巨细胞瘤治疗药物安加维®地舒单抗在中国获批
2019-05-27 小M MedSci原创
2019年5月27日,上海——安进中国今日宣布,安加维®(英文商品名XGEVA®,通用名:地舒单抗注射液,Denosumab Injection)获得国家药品监督管理局批准。
2019年5月27日,上海——安进中国今日宣布,安加维®(英文商品名XGEVA®,通用名:地舒单抗注射液,Denosumab Injection)获得国家药品监督管理局批准,用于治疗不可手术切除或者手术切除可能导致严重功能障碍的骨巨细胞瘤,包括成人和骨骼发育成熟(定义为至少1处成熟长骨且体重≥45 kg)的青少年患者。2018年,安加维®被列入临床急需境外新药名单(第一批),进入国家药品监督管理局快速审评通道。此次获批使得安加维®成为首个,也是目前唯一一个用于骨巨细胞瘤治疗的药物,为患者带来了控制疾病进展、改善生活质量的创新治疗选择。
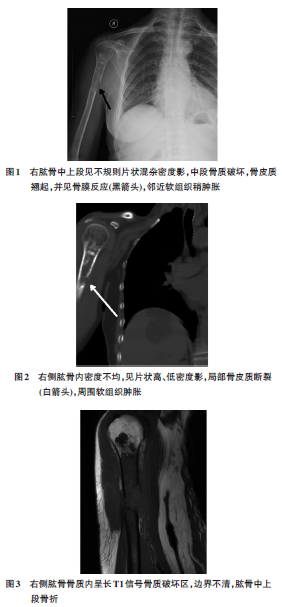
骨巨细胞瘤是一种组织学上良性,但常常具有侵袭性的骨骼肿瘤,好发于20~40岁青壮年人群,女性发病率略高于男性,约占56.4%。从全球来看,骨巨细胞瘤约占所有骨原发肿瘤的4%-5%,与欧美人群相比,在中国更为常见,约占所有原发骨肿瘤的20%。尽管绝大多数骨巨细胞瘤为良性肿瘤,但若不进行治疗,经常引起受影响的骨骼完全损坏,导致骨折、关节功能障碍或截肢。
骨巨细胞瘤由表达RANKL的基质细胞和表达RANK受体的破骨细胞样巨细胞组成,其发病机理是RANKL的过度表达引起肿瘤生长和骨质破坏。RANKL是破骨细胞形成、发挥功能和生存所必需的跨膜或可溶性蛋白;破骨细胞负责骨吸收,从而调节骨钙释放。安加维®是一种人免疫球蛋白G2(IgG2)单克隆抗体,对RANKL具有高特异性和亲和性。 RANK 受体信号传导促进了骨质溶解和肿瘤生长。安加维®通过与RANKL结合,阻止其激活破骨细胞、破骨细胞前体和破骨细胞样巨细胞表面的RANK,从而达到抑制肿瘤生长和减少骨破坏的目的。
北京积水潭医院骨肿瘤科主任、中国临床肿瘤学会肉瘤专家委员会主任委员牛晓辉教授表示:“根据一项骨巨细胞瘤中国发病率研究报告,中国骨巨细胞瘤年发病率估算为1.49~2.57例/100万,整体来说是一种非常少见的疾病。当前的治疗方法主要包括手术与放疗。手术是骨巨细胞瘤主要的治疗方法,但术后复发率较高。根据不同研究报道,骨巨细胞瘤刮除术后的复发率为15%~45%。放疗在一定程度上可以控制肿瘤的生长,但存在放疗后并发症及潜在的肉瘤样恶变风险。对于那些不可手术切除或手术切除会带来严重功能损伤的患者来说,此前并无获得中国监管部门批准的有效治疗药物。地舒单抗的获批意味着中国骨巨细胞瘤患者期盼以久的创新治疗选择终于到来,其抑制肿瘤生长和减少骨破坏的双重作用以及良好的耐受性将为患者带来疾病治疗获益和生活质量的提高。”
安加维®此项适应症获批是基于两项开放标签的试验研究结果,针对复发性、无法切除或计划的手术切除很可能会造成严重功能障碍的骨巨细胞瘤患者。2017年在欧洲肿瘤内科学会(ESMO)年会上发表的该研究最新分析结果显示,在可以手术切除的患者中,80%的患者接受新辅助地舒单抗治疗后得到改善:44%接受了对功能影响较小的手术,37%避免了手术。在无法手术切除的患者中,地舒单抗带来了有效的长期疾病控制,5年无进展生存(PFS)率为88%。
安进公司副总裁兼亚太区总经理温陈佩茜表示:“作为首个,也是目前唯一一个在中国获批的骨巨细胞瘤治疗药物,安加维®的到来对罹患这一少见疾病的患者来说,意义非同一般,尤其是无法进行手术或手术会带来严重伤残的患者,我们为此感到振奋。同时,安加维®是安进为中国患者带来的第一个肿瘤治疗药物,它将为我们在中国市场的发展注入新的动力,也为肿瘤领域的开拓奠定基础。未来,我们将继续致力于服务患者,深耕重大疾病领域,针对未被满足的医疗需求,为中国患者带来更多的创新疗法,为健康中国的建设贡献我们的力量。”
安加维®此前已获得美国食品药品监督管理局(FDA)、欧盟委员会(EC)等机构的批准。
关于骨巨细胞瘤
骨巨细胞瘤是一种局部侵袭的良性肿瘤,好发于20-40岁的青壮年3。在中国,骨巨细胞瘤大约占所有原发骨肿瘤的20%5。
骨巨细胞瘤多发生于四肢长骨,极少情况会出现肺转移。尽管骨巨细胞瘤病程进展缓慢,但经常伴随严重的骨痛、肿胀、行动能力丧失和病理性骨折。在安加维®获批之前,一直未有药物获批用于骨巨细胞瘤的治疗。对于可切除的骨巨细胞瘤,患者的主要治疗选择是外科手术。然而,部分患者需要接受例如关节切除、截肢这类导致术后功能明显受损的手术。相当一部分患者会在初次手术后复发,复发后会变得更加难以治疗,也可能发生转移。
关于安加维®
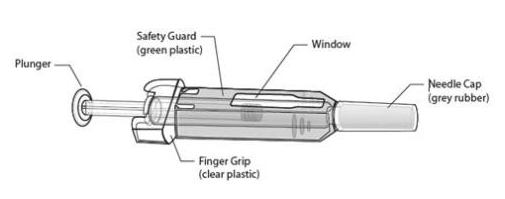
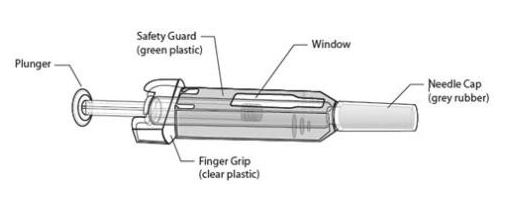
安加维®(英文名XGEVA®,通用名: 地舒单抗注射液,Denosumab Injection),是一种人IgG2单克隆抗体。
安加维®与RANKL结合,RANKL是破骨细胞形成、发挥功能和生存所必需的跨膜或可溶性蛋白;破骨细胞负责骨吸收,从而调节骨钙释放。类似地,骨巨细胞瘤由表达RANKL的基质细胞和表达RANK受体的破骨细胞样巨细胞组成,RANK受体信号传导促进了骨质溶解和肿瘤生长。安加维®可阻止RANKL激活破骨细胞、破骨细胞前体和破骨细胞样巨细胞表面的RANK。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗药物#
31
#细胞瘤#
30
#骨巨细胞瘤#
44
#巨细胞#
37
#安加维#
18